California May Extend 5150 Power to More Clinicians
State senators pass a bill to allow mental health professionals put people in involuntary psychiatric holds. Ketamine clinics are proliferating across the US, with mixed results. And more.


Wednesday, January 31, 2024
By Courtney Wise

Greetings, MindSite News Readers. In today’s Daily: California senators pass a bill that would allow more mental health professionals to place people on involuntary psychiatric holds. Canada has again delayed making medical aid in dying available to the mentally ill. Ketamine clinics are proliferating across the USA, with mixed results. Plus, an in-depth interview with author Antonia Hylton about her new book on the history of Maryland’s “Jim Crow asylum.”
California advances bill giving more clinical professionals the power to place psychiatric holds
Under a well-known section of California law known as Section 5150, people who are considered a danger to themselves or others, or are “gravely disabled,” can be involuntarily taken to a hospital for up to 72 hours for a psychiatric evaluation. But who gets to make this decision?
Under current law, it’s police officers, members of mental-health crisis teams and those in charge of treatment facilities, along with some other county-designated officials. Non-designated psychiatrists or therapists don’t have that power.
This week, the State Senate passed a bill that would expand those authorized to issue a mental health hold to psychiatrists, psychologists, clinical social workers, licensed marriage and family therapists and clinical counselors. The bill’s author, State Sen. Aisha Wahab (D-Hayward), told CalMatters that she wants to put mental health professionals – rather than police officers – in the driver’s seat. “The problem here is that the individuals that are actually trained in this science, in this profession, in this industry, are not empowered enough to make the best decision for the people they work with the most,” she said.
A staffer for Wahab further explained to MindSite News that currently, most counties limit the clinical professionals who are given this power to people who are employees or contractors of the county. Under the proposed legislation, any mental health professional – including those who are not employees or contractors – would be able to place a person on an involuntary hold.
The bill passed with bipartisan support, but it has its critics. Disability rights activists argue that giving more officials the power to detain mentally ill people may deter them from getting help and could erode their trust in the very people they turn to for help. Detractors also brought up logistical concerns. When it comes time to transport someone to the hospital, “we think law enforcement is going to get called, and that’s how it will play out in real-time,” Debra Roth of Disability Rights California testified before the Senate Health Committee.
Wahab says the hope is that if a person experiences a mental crisis with their therapist or social worker, their established relationship will enable the ill person to accept the hold. That expected level of trust can make the process less confrontational – and less dangerous – she added. Broader partnerships with ambulance and crisis services could also help.
Canada delays extending medical aid in dying to the mentally ill
After navigating years of severe depression without relief, Jason French anxiously anticipated March 17, 2024. That’s the day Medical Assistance in Dying was to become available to Canadian adults with mental illness – as it currently is for Canadians with incurable physical ailments that cause intolerable physical pain. But on Monday, Canadian officials announced a new delay, with no new date set for when the law might expand to those with incurable mental illnesses, the New York Times reported.
French had attempted suicide twice before and planned to pursue medically-assisted death. “My goal from the start was to get better,” French told the New York Times last year. “Unfortunately, I’m resistant to all these treatments and the bottom line is, I can’t keep suffering. I can’t keep living my life like this.”
Canadians who are chronically and terminally ill have had the right to end their own lives with assistance from a doctor since 2015, but the plan to extend the program to people with mental illnesses has divided Canadians. Health offficials say there aren’t enough licensed psychiatrists to assess whether patients with mental illness are lucid when they request a medically-assisted death.
“The system needs to be ready, and we need to get it right,” Health minister Mark Holland told reporters. “It’s clear from the conversations we’ve had that the system is not ready, and we need more time.”
Opponents of the law argue it will undermine suicide prevention efforts and discourage the country from providing the resources that are needed to treat mental illness. Those in support of the expansion say that no one should be made to suffer and that people in psychic pain that can’t be eased shouldn’t be forced to keep suffering.
Debates over ketamine – the “wild west” of mental health treatments – continue
Fifty years ago, ketamine was largely for folks raging against the machine – hard to find and radical to take. These days, it’s gone mainstream, with hundreds of for-profit ketamine clinics operating around the country. Patients at these clinics can take the drug for a range of mental health issues, including obsessive-compulsive disorder, depression, and anxiety. Ketamine isn’t approved for these uses but it is cleared as an anesthetic, so the off-label treatments are legal. They’re also expensive. Since ketamine isn’t approved for mental illness, insurance rarely pays for the therapy which can cost $600 to $1,000 per session.
Two years ago, Sarah Gutilla was so depressed she was contemplating suicide. She and her husband scraped together $600 to cover an infusion of intravenous ketamine therapy at Ketamine Clinics Los Angeles, and Gutilla felt an immediate difference. “The amount of relief I felt after the first treatment was what I think ‘normal’ is supposed to feel like,” she says. “I’ve never felt so OK and so at peace.”
But a lack of clinical guidelines has turned ketamine into “the Wild West,” said Dustin Robinson, managing principal of a venture capital firm that invests in hallucinogenic treatments. Doses and prescribing practices vary widely. Some providers like to start with low doses and gradually increase in strength. Others prefer to administer doses large enough to induce hallucinations. As MindSite News reported last year, some clinics start with two infusions a week for three weeks; another infuses patients five days in a row – a regimen one psychiatrist described as “scary.” And companies like Mindbloom offer ketamine therapy at home, with the medicine taken as a tablet that dissolves under the tongue.
The drug drew attention for contributing to the death of Friends star Matthew Perry, who had received ketamine via infusion therapy one week before his death. As it turns out, that ketamine didn’t contribute to his death – but the high-dose ketamine he took with an opioid and a sedative on the day of his death did. Sam Mandel, co-founder of Ketamine Clinics Los Angeles, told the Hollywood Reporter that “there is zero correlation between what happened with Matthew Perry and the therapeutic clinical use of ketamine for mental health.”
But is that really the case? Perry might have gotten his high dose ketamine from the street, but what’s to stop people from filling multiple prescriptions or exceeding recommended dosing when they take the drug at home?
Mandel says patients must choose providers carefully if they want to mitigate their own risk. He suggests using clinics (like his, of course) that provide ketamine infusions as their primary business, that are equipped with hospital-grade monitoring equipment and that employ clinicians with expertise in both mental health and anesthesia.
In other news…
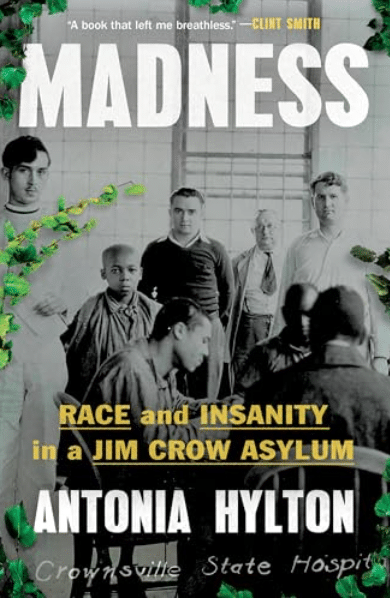
There’s much more to learn about the place once known as the Hospital for the Negro Insane of Maryland. In her book, MADNESS: Race and Insanity in a Jim Crow Asylum, journalist Antonia Hylton offers an extensive history of the institution – and the abuse and exploitation it perpetrated. In an interview with NPR’s Fresh Air, Hylton said that many of those committed were not, in fact, ill – like the man who was locked up for having a British accent despite being from London.
“This was about getting access to free Black labor. In the hospital records [there] was a lot more commentary about the labor and the amount of products that patients could produce than…about mental health care outcomes,” she said. “Tells you a lot about a facility’s priority.” A NYT review of the book can be found here.
In a guest column for the Washington Post, three psychiatrists implore the medical community to train future doctors in how to support suicidal patients. Primary care doctors are often the first point of contact with someone contemplating suicide, wrote Rodolfo Bonnin, Leonard M. Gralnik and Nathaly Shoua-Desmarais. They point to evidence that “roughly 44 percent of adults who died by suicide worldwide had visited their primary care provider within one month of their death.” Many physicians miss signs of suicide because they aren’t trained to spot them, the authors noted. They may also be too uncomfortable to talk about suicide or have enough time to work with patients who need them.
Eyes are again turned toward Mississippi, where James Tatsch recently died in a jail cell, despite not being charged with a crime. He had been detained for 12 days, awaiting mental health treatment. Read more on this story at Mississippi Today.
If you or someone you know is in crisis or experiencing suicidal thoughts, call or text 988 to reach the 988 Suicide & Crisis Lifeline and connect in English or Spanish. If you’re a veteran press 1. If you’re deaf or hard of hearing dial 711, then 988. Services are free and available 24/7.
Recent MindSite News Stories
The Night Parade: A genre-bending memoir that helps reshape the cultural narrative on bipolar illness and grief
Jami Nakamura Lin has written a rich, exquisitely illustrated memoir that expands the cultural narrative on mental illness and grief.
A Former Hotline Counselor ‘Hands the Mic’ to Call-takers to Amplify Their Voices
The author of a survey of crisis hotline counselors talks about his experiences and why he wanted to tap into the wisdom of the people who answer calls to 988.
988-Hotline Counselors Air Concerns About Lack of Training, Rushed Calls
A newly released report, based on responses from 47 crisis counselors, explored variations in their training and work experiences. The first-of-its-kind survey raised raised the voices of 988’s workforce and surfaced some interesting snapshots.
If you’re not subscribed to MindSite News Daily, click here to sign up.
Support our mission to report on the workings and failings of the
mental health system in America and create a sense of national urgency to transform it.
For more frequent updates, follow us on Facebook, Twitter and Instagram:
The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.
Copyright © 2021 MindSite News, All rights reserved.
You are receiving this email because you signed up at our website. Thank you for reading MindSite News.
mindsitenews.org

Mental health can't wait.
America is in a mental health crisis — but too often, the media overlooks this urgent issue. MindSite News is different. We’re the only national newsroom dedicated exclusively to mental health journalism, exposing systemic failures and spotlighting lifesaving solutions. And as a nonprofit, we depend on reader support to stay independent and focused on the truth.
It takes less than one minute to make a difference. No amount is too small.
The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.