The Addiction Story Everyone Should Hear
What if everyone with a drug problem was involved in a free comprehensive, long-term recovery program? Plus, Arizona’s 988 success story. More than half of mental health appointments are now remote. And more.


February 19, 2024
By Don Sapatkin

Good Monday Morning! We all (well, most of us) like holding hands, right? The Washington Post tells why, biologically speaking. And in today’s upbeat Daily: A model for recovery from addiction we’d like to see replicated all over.
In other news: An Arizona template for how 988 was meant to work. Telemental health is huge. New York City sues social media companies over youth mental health. And U.S. overdose deaths from smoking drugs soared while those from injecting plummeted. Plus: If you’re into self-help books, why not get the ones that therapists are reading?
“The addiction story we don’t hear enough”
Watching 20 women with felony records and a history of drug use graduate from a program called Women in Recovery in a boisterous ceremony, New York Times columnist Nicholas Kristof’s imagination soared: “What if everyone with a drug problem who was caught up in the criminal justice system had access to a comprehensive and long-term recovery program like this?” Then he dreams a bit more: “What if high-quality treatment programs were available free to all 48 million Americans over the age of 12 who, according to federal estimates, have a substance use disorder involving drugs, alcohol or both?”
Kristof, if you’re unfamiliar with him, is a brilliant journalist who won Pulitzer Prizes for his coverage of China and of the genocide in Darfur. But it’s his opinion articles, to which he brings a combination of deep compassion, intensive reporting and a never-ending search for solutions, that move me the most. Like when he traces the lives of the kids on his No. 6 school bus in the rural, working class town in Oregon where he grew up, a quarter of whom are now dead, mostly from drugs, suicide, alcohol or reckless accidents. His latest piece is part of the series “How America Heals,” in which he examines the interwoven crises devastating working-class America and explores paths to recovery.
Kristof has been visiting and following Women in Recovery, a diversion program for women in the Tulsa, Oklahoma area who would otherwise face prison for drug-related offenses, for a decade (and spoke at two graduations). Although not a panacea, he calls it “the single best program I know of to fight substance use,” with a simple lesson to offer: “Addiction is not hopeless.” About 70 percent of women who start the program complete it, and of those who graduate, just 3.7 percent have returned to prison within three years of graduation. About 130 women are in the program at any given time. What’s unusual about Women in Recovery and helps it succeed where many of the nation’s 17,000 substance abuse clinics do not, Kristof believes, is that it lasts 18 months for a typical participant, far longer than most recovery programs. And it’s comprehensive, aiming to restore a woman’s mental health, reunite her with her children, teach her a skill, get her a job, coach her on financial literacy and knit her back into a community. The women have an average history of 15 years of addiction, and it takes a while for them to rewire their brains.
One of the recent graduates was 27-year-old Katelyn Fullbright (above), who had been a star athlete and an A student early in high school before heading into trouble, and, at 16, a boyfriend who introduced her to cocaine and meth. Small amounts at first. And then “just dating bad boys. That’s definitely a fault of mine,” she said. Fullbright began selling drugs to finance her habit, married a man who also was in the drug world, was arrested with a cache of drugs and faced a 10-year prison sentence. She got into Women in Recovery but didn’t like it: for the first few months, women are virtually under house arrest. She ran off with her husband and, when she was arrested a year later, was sent to prison where “I got high all the time” in what she described as an “inmate-run” facility where drugs were widely available. Her mother convinced her to apply from prison to re-enter Women in Recovery.
The program helped her get a divorce, she joined Narcotics Anonymous, which she said was helpful, and gradually earned more freedom. Finding employment and housing are difficult for people with felony convictions, but Women in Recovery has built a record of success and won the trust of the business community, with many Tulsa companies even offering apprenticeships to graduates. An oil company hired Fullbright as an administrative assistant, and she likes it so much that she’s thinking about going back to school to become a petroleum geologist. Looking for an apartment, she told her story to a woman in a rental office, who said she loved Women in Recovery and offered her an apartment.
“When I write about addiction, it’s normally about the overdoses, the heartache, the burden on families,” Kristof says at the end of the piece. “So it’s exhilarating to write about a program associated with pride, joy and success. It’s a reminder that we have solutions, however imperfect, and we as a nation have resources to scale them up. I dream of a time when there are rigorous, evidence-based programs such as this all across America, for men as well as women, sprinkling hope for millions of families desperate for answers.” (See also: 48 Million Americans Live With Addiction. Here’s How to Get Them Care That Works.)
This is what mental health crisis care should look like
In the year and a half since 988 launched, we’ve all read stories about how the expanded national suicide and crisis hotline, despite its success in dramatically increasing the number of calls, has a very long way to go. So I was surprised – thrilled, frankly — to catch PBS NewsHour’s report (9:34, with a full transcription) about a call center, and a state, that are fulfilling much of the vision of what 988 was intended to eventually become: one (critical) part of a mental health crisis care continuum that seamlessly coordinates among emergency counselors working by phone/text/chat, round-the-clock mobile mental health teams in the community, and brick-and-mortar centers that provide safety and stabilization for up to a day for people in extreme distress, and then work to connect them to longer-term treatment.
A nonprofit called Solari is contracted by the state to run one of the largest crisis call centers in the country by volume in Tempe, Arizona, outside Phoenix. When Raquel Medina’s obsessive-compulsive disorder and anxiety overcame her six months ago, eventually leading to thoughts of suicide for several nights, she texted 988.The response was instantaneous. The counselor “stayed up with me for a couple of hours in the middle of the night just talking with me, texting. We went back and forth. And I kind of explained everything, and she was really supportive and really understanding,” Medina told reporter Stephanie Sy. The crisis care specialist even followed up later and connected her to a list of therapists that could take her insurance. Hotline counselors’ goal is to stabilize the person in crisis remotely, and Solari does so nearly 80% of the time. If the caller needs more help, an in-person team is dispatched to talk with them.
If still more is needed, the team transports them to a crisis stabilization unit that’s designed to be a safe place for people in severe psychiatric distress. They can stay there up to 23 hours, which is enough time for most to become stable with the help of a team of physicians, nurses, and behavioral health specialists who may consult with social service workers and peer specialists. For people who were brought in by police, the handcuffs quickly come off. “It’s important because we need to signify that you’re coming into a place for treatment,” said Thereas Costales, Arizona Medical Director for Connections Health Solutions. They may be “just very, very depressed and having these strong suicidal thoughts and urges, maybe just attempted suicide,” she said, “and they’re not combative.”
Costales says the state’s system is unique, built out to treat severely mentally ill individuals in community settings. Its three components — hotline, mobile crisis teams and stabilization centers — provide a continuum of care 365 days a year, with no break for holidays. Twenty states offer 24/7 mobile crisis teams but the full continuum of care, when it’s available, typically is an 8-to-4 weekday-only operation often manned by volunteer services, said Andrew Medina, the state’s Medicaid crisis administrator. “But, here in Arizona, for well over 30 years, we have created a system that’s available to any Arizonan whenever they need the help.”
In other news…
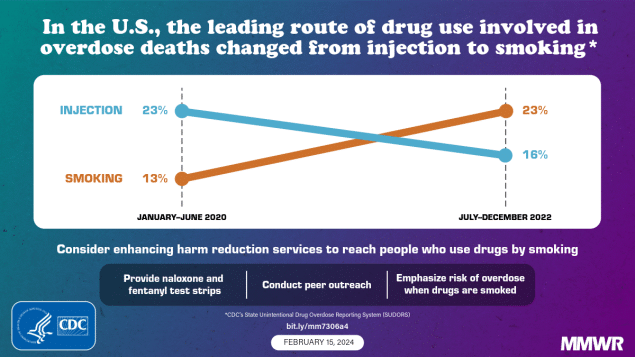
Overdose deaths involving smoking were up sharply while injecting was down between 2020 and 2022, according to an analysis of data from 27 states and the District of Columbia in the CDC’s Morbidity and Mortality Weekly Report. Researchers attributed the dramatic shift, which made smoking the top route for administering illicit drugs, to the transition from shooting heroin to smoking fentanyl and its analogs. The latter were involved in nearly 70% of the estimated 109,000 drug overdose fatalities in 2022. The percentage of deaths with evidence of injection decreased 29%, while those with signs of smoking, which can intensify drug effects and raise overdose risk, increased 74%. Snorting rose, too. Other motivations for the shift from needles to inhaling cited by the authors were fewer adverse health effects such as abscesses, reduced cost and stigma, a sense of more control over the drug quantity consumed per use, “and a perception of reduced overdose risk among persons who use drugs.”
More than half of mental health appointments are now remote, mainly via video conference, the Washington Post reports. A brief and fully paywalled study of 277 million outpatient visits by 9 million veterans in Annals of Internal Medicine found that 55% of mental health visits were done via telehealth. An unrelated secret shopper study in JAMA Health Forum found that 80% of mental health treatment facilities accepting new patients said they offered telehealth services. Availability did not vary according to diagnosis but did by type of service (97% of those that offered telehealth did so for counseling, 77% for medication management and 69% for diagnostics) and geography.
New York City sued TikTok, Instagram, Facebook, Snapchat and YouTube, alleging that the social media platforms harm young people’s mental health, serve as venues for bullying, and are designed to be addictive, CNN reported. The complaint calls on the companies to change their practices and pay for youth mental health education, prevention and treatment services. Officials said the city spends about $100 million a year on youth mental health programs. Its Education Department and public hospital system are also part of the lawsuit, which was filed in a California state court. Hundreds of school districts, as well as states, municipalities and families have sued social media companies over the youth mental health crisis, but New York’s complaint got an unusual amount of international press.
If self-help books all seem the same, try the ones that therapists read themselves. The New York Times suggests six. First on the list: “The Book of Joy: Lasting Happiness in a Changing World,” by the Dalai Lama, Desmond Tutu with Douglas Abrams. “Through their dialogue, which is punctuated with laughter and tears, the Dalai Lama and Archbishop Tutu teach readers how to cultivate joy and work through difficulties like illness and despair,” the Times writes of the 2016 book.
Others on the therapists’ list: The Happiness Trap (Russ Harris), Tattoos on the Heart: The Power of Boundless Compassion (Gregory Boyle), The Artist’s Way (Julia Cameron), Homecoming: Healing Trauma to Reclaim Your Authentic Self (Thelma Bryant), and The Power of Character Strengths (Ryan M. Niemiec and Robert E. McGrath).
If you or someone you know is in crisis or experiencing suicidal thoughts, call or text 988 to reach the 988 Suicide & Crisis Lifeline and connect in English or Spanish. If you’re a veteran press 1. If you’re deaf or hard of hearing dial 711, then 988. Services are free and available 24/7.
Recent MindSite News Stories
A San Francisco Program Helps Older People Manage Their Hoarding Behavior – and Stay Housed
Every year, 20 or more elderly San Francisco renters are threatened with eviction because of their hoarding disorder. A unique peer-support program helps them make changes – and keep their apartments. Continue reading…
Help! I Don’t Like My Child
A divorced father can’t figure out why he no longer enjoys his teen daughter’s company. Find out what Dr. Greenberg advises. Continue reading…
The Night Parade: A genre-bending memoir that helps reshape the cultural narrative on bipolar illness and grief
Jami Nakamura Lin has written a rich, exquisitely illustrated memoir that expands the cultural narrative on mental illness and grief. Continue reading…
If you’re not subscribed to MindSite News Daily, click here to sign up.
Support our mission to report on the workings and failings of the
mental health system in America and create a sense of national urgency to transform it.
For more frequent updates, follow us on Facebook, Twitter and Instagram:
The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.
Copyright © 2021 MindSite News, All rights reserved.
You are receiving this email because you signed up at our website. Thank you for reading MindSite News.
mindsitenews.org

The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.