Working to Fend Off Dementia
Mild cognitive decline may be a precursor to dementia, but you can take steps to stop or delay its progress. Psychologists work with Hollywood and indies to dispel myths about mental illness. And more.


March 5, 2024
By Courtney Wise

Greetings, MindSite News Readers! In today’s Daily, we look at mild cognitive decline and what research says about possible ways to stop or slow its progress. In other news, the entertainment industry makes greater efforts to accurately portray mental illness onscreen, cyberattacks on a mental health care provider wreak havoc, and why so many mental illnesses overlap. Plus, the benefits of saying no.
Treating mild cognitive impairment may stop or slow its progress to dementia
More than a little forgetfulness, mild cognitive impairment (MCI) is a decline in memory, thinking and judgment that muddles one’s ability to function. For some, but not all, it may even be a precursor to dementia. MCI affects far more people than may realize, with up to 92 percent of MCI patients going undiagnosed, according to research. It’s such a subtle condition that even though many MCI patients recognize their cognitive and memory lapses, it’s easy enough to attribute the changes to stress, regular aging or something else. Jonel Dershem was just 50 years old when she and her son began to notice slips in her memory. It was 2016 and the obstetrician – and primary breadwinner for her household – had just finished breast cancer treatment. She and her doctors assumed her memory challenges were due to stress and the after-effects of chemotherapy. “I kept blowing it off,” Dershem told the Washington Post. “I didn’t want there to be any serious problems.”
But “blowing off” getting checked can mean MCI getting worse. If caught early, however, new medications like lecanemab (brand name Leqembi) may help. The drug was federally approved just last year to treat MCI and early Alzheimer’s disease. It works by reducing the buildup of amyloid beta, the brain protein associated with Alzheimer’s. But clinical trials have shown it can only moderately slow dementia’s progress: It has not been shown to recover cognitive or memory decline that was lost. Visiting your doctor and being specific about your issue is crucial to catching MCI early and getting appropriate treatment. Call her right away if you begin to notice trouble with memory, retaining new information or even missing social cues you mastered in the past.
If you’re bookish (like me) and want to get a head start on your doctor’s visit, consider taking the Self-Administered Gerocognitive Exam (SAGE) at home. Save test results to help drive the appointment and conversation about what’s next with your physician. And most important, take someone you trust to all medical appointments with you. That person can serve as emotional support as they record critical information from the appointment and ask questions or explicitly advocate on your behalf. Karen Sandone of Doylestown, Pennsylvania, told the Post she learned the urgency of attending medical appointments with her husband the hard way: She let him go on his own and accepted his account of what happened when he returned home. “When he came back home, he said everything was fine,” Sandone said. But then, she looked at the evaluation herself. “I was like, ‘Oh my goodness, how could he say everything was okay?’ I didn’t realize that he couldn’t understand or remember what [the doctor] was saying.”
In the event you or a loved one receive an MCI diagnosis, take it seriously and know there are steps you can take to support your brain. Many of them are healthy actions to take now, even if MCI isn’t a concern. Make sure your other diseases are carefully managed and monitored, exercise regularly, get a full night’s sleep, limit alcohol intake and stress, and eat a balanced diet. The benefits of a healthy diet cannot be understated. Researchers found that changes like trading saturated and trans fats (in foods like beef ribs, sausage, butter and commercially baked cookies and cakes) for unsaturated fats (think seafood, walnuts and olive oil) may slow cognitive decline and reduce the risk of Alzheimer’s disease.
Research also suggests that turmeric has anti-inflammatory properties that have the potential to shrink amyloid beta plaques and prevent or slow the progression of Alzheimer’s disease. In addition, studies suggest that walking 3,800 steps a day can help reduce the risk of Alzheimer’s by 25% (and at 10,000 steps, by 50%), as well as lowering the risk of high blood pressure, heart disease and stroke. After 11 months of treatment, doctors told Dershem – who has been exercising regularly, eating healthy meals and spending time with the family – that they haven’t seen further mental decline. “I’m just trying to do everything I can,” she said.
Psychologists work to dispel myths about mental illness in TV series and film

Eight years ago, Helen Hsu barely even watched TV. She wasn’t against it; the psychologist was just so busy providing clinical care to low-income children and families and overseeing a public school–based counseling program that TV was hard to squeeze into her schedule. But her reputation as an expert in adolescent mental health preceded her, prompting Netflix producers to call. Their show, 13 Reasons Why, based on a novel of the same name, follows the story of a high school freshman and the thirteen reasons she died by suicide. For the producers, consulting with an expert in adolescent and multicultural mental health was vital not only to honor the original story, but to protect the health and safety of viewers. Hsu jumped at the chance, she told the American Psychological Association. “I thought, here’s another opportunity to get information to an audience that’s far larger than what I could ever do academically.”
Hsu’s story is common as media makers and mental health experts partner to ensure stories accurately reflect the reality of mental illness. In doing so, harmful myths about mental health are overturned, characters made more authentic, and in the best cases, the mental health of viewers is elevated. Though lots of criticism was (reasonably) lobbed at Netflix for the show, especially for a graphic suicide scene that was later removed, Hsu said the show is linked to an increase in calls to crisis lines, greater male awareness of sexual assaults, and important conversations between parents and children about mental health.
“Storytelling has always been a way for us to find healing, to better understand our own identities and one another, to understand differences, to be able to safely and more confidently talk about the things that, under other circumstances, might feel too vulnerable, unsafe, personal,” said Drea Letamendi, a clinical psychologist who advises the gaming, visual effects and film industries. “So we can use the media to talk about very impactful, real psychological topics and increase their awareness. And in many ways, this increases people’s interest and buy-in in psychological science, which is really important right now for our field.” Media makers agree that their programs reflect and affect pop culture, too. “There is a lot our audience can and does learn from the content they watch, and it shapes norms and it changes the conversation,” said Noopur Agarwal, MTV Entertainment Studios’ vice president of social impact.
Some shows have even taught viewers new coping skills for managing stress, Agarwal said. Seventy-five percent of those who watched the Paramount+ drama Wolf Pack said the show introduced them to new coping tools. As its characters deal with attacks from a supernatural creature, they employ ‘Lion’s breath,’ a wide-mouth, tongue-out breathing exercise that helps real-life people manage stress and anxiety. Even preschool viewers benefit from psychologist-informed TV. Temple University developmental psychologist Kathy Hirsh-Pasek said she’s seen evidence of Sesame Street’s impact throughout her years consulting for the show. According to research, children who watch more Sesame Street have been shown to be better problem-solvers who think about challenges in a healthier way. “They would give more tries,” Hirsh-Pasek said. “They wouldn’t just give one try and quit.”
Why saying no when you need to is so important
Serving up endless cups of coffee almost stopped writer Leslie Jamison from writing her first book. Okay – I’ve employed some hyperbole there, but it’s safe to say her book was severely delayed due to her fear of saying no. She writes in the New York Times that when she initially set out to complete the book, she was employed at a Midwest coffee shop by a boss that always asked her to stay late or take on another shift. “If I said no, I worried that I would be leaving her in a jam,” she wrote, “or that she might decide I wasn’t worth keeping on the staff at all. (My skills in the kitchen hardly justified my presence.)” So, saying no is something she just didn’t do. The book wasn’t writing itself, either.
Frustrated, she vented to her stepfather, expecting sympathy. Instead, he simply said, “She has the right to ask the question, and you have the right to say no.” That revelation changed everything, Jamison said.
There’s this fear of saying no to people that prevents many of us from honoring ourselves. When that happens, it’s actively harming us. Like the writer, I let myself be locked into a years-long gym membership because I didn’t want to hurt the salesperson’s feelings. I was a college student, unemployed, and not yet 20 years old. The salesperson got a commission and I got bad credit. It was my first memorable lesson in the importance of saying no.
To help herself confront her fear of ‘no,’ Jamison says she turned to journaling. She likened it to habit tracking that she could reference for a record of her changed (or unchanged) behavior. “It was as if, in their accumulation, they could create a meaningful text: the story of learning to live a different way,” she wrote. “As I gathered more of these noes, I learned that, even after I’d uttered the word, the world continued just as it always had…[and] instead of lamenting the ghost limb of what I wasn’t doing, I could acknowledge that every refusal was making it more possible to do something else.”
In other news…
Anxiety and depression; PTSD and substance use disorder: Why do so many mental illnesses overlap? In sum, scientists still don’t know. There’s a lot of debate among them. with many arguing genetics are responsible. Mine and your propensity for mental illness depends on the ‘general psychopathology factor’ or ‘p factor,’ which accounts for nearly 40 percent of our risk, they say. Why this argument? Well, science has learned that many illnesses share some of the same genes. For instance, ADHD, PTSD, depression and obsessive-compulsive disorder have a number of genes in common. Schizophrenia and bipolar disorder share a set of genes, too. But, there is still much to understand: The p factor in each of us doesn’t mean mental illness in all of us. Researchers told Scientific American they hope future studies leave room for an examination of multiple conditions at once, rather than studies focusing on one illness in isolation.
A February 21 cyberattack affecting Nashville-based tech company Change Healthcare is still causing serious problems for mental health and medical providers. Patients are having trouble getting prescriptions filled and insurance reimbursements are delayed, causing practice owners to worry about how to pay their staff. Ann-Marie Foster, president and CEO of mental health and substance-use nonprofit Phoenix House, told Crain’s New York Business that her company has 2,700 insurance claims waiting to be processed, accounting for $560,000 in billable services. “We need this to be rectified sooner rather than later,” she said. “Because in a very short window, we could have some serious cash flow issues, and that means being [unable] to pay our vendors and meet payroll.”
Yoga functions as a form of moving meditation for this Black yogi: Quamay Sams is a yoga instructor with the digital platform Glo. He told Yahoo News that the practice gave him a new career and helps him to manage his mental health. “I have ADHD but also suffer from anxiety [and] depression. I’ve also been diagnosed with bipolar II,” he said. “So learning how to, I wouldn’t say quiet the noise, but just learning how to navigate the fact that I have to, something’s constantly going on in my mind, and being able to kind of create some space and separate from it for a moment to just realize that it doesn’t have to dictate everything that I do and feel has been a blessing.”
If you or someone you know is in crisis or experiencing suicidal thoughts, call or text 988 to reach the 988 Suicide & Crisis Lifeline and connect in English or Spanish. If you’re a veteran press 1. If you’re deaf or hard of hearing dial 711, then 988. Services are free and available 24/7.
Recent MindSite News Stories
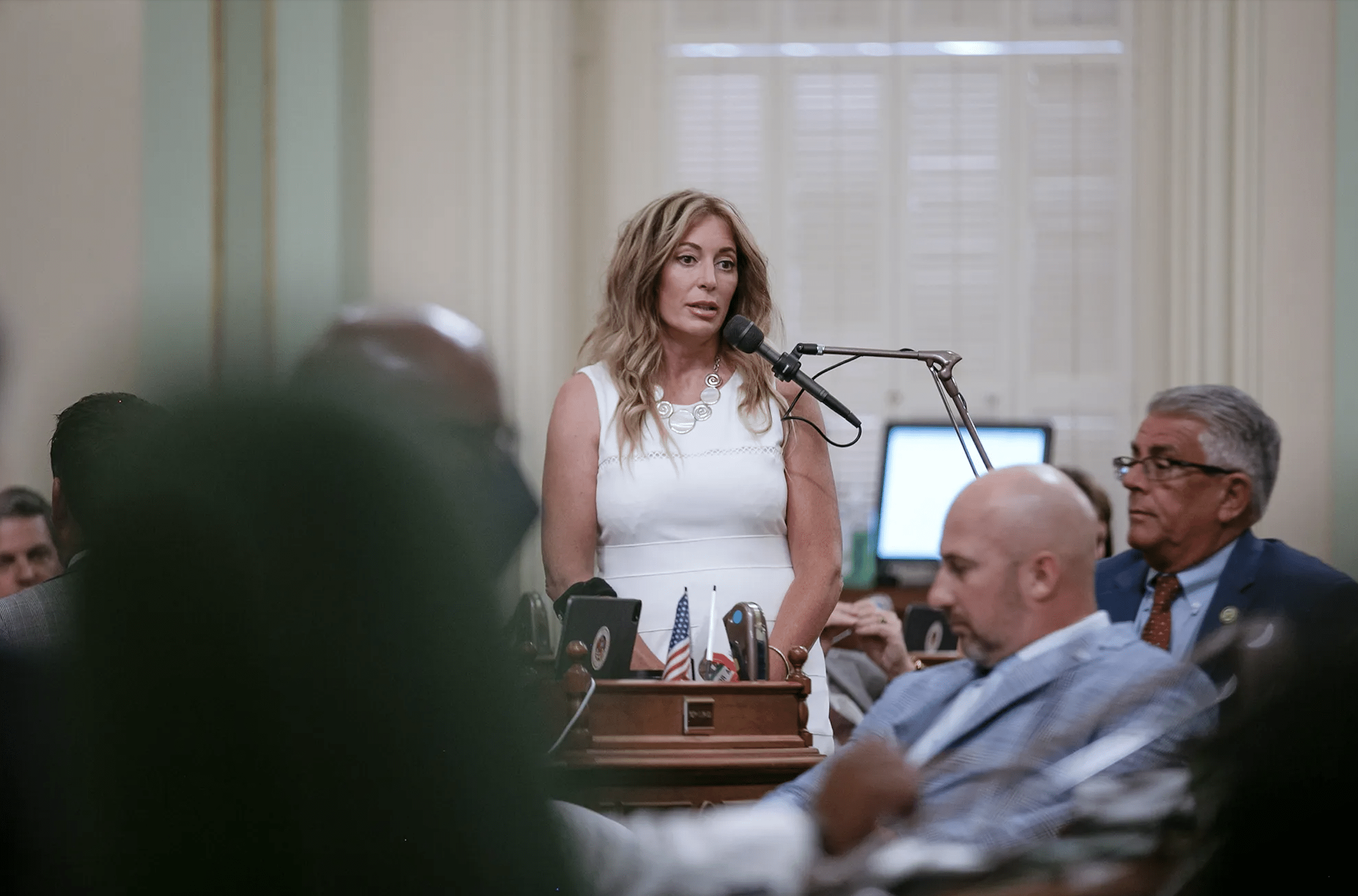
Can Prop. 1 Address California’s Trifecta of Mental Health Crises? Voters Are About to Decide
As voters prepare to pass judgment on Proposition 1, MindSite News asked six key players in the state’s constellation of mental health services to weigh in on its likely impact. Will it finally succeed in helping the state address its mental health and homelessness crisis? Continue reading…
How psychedelic drug therapy became a rare bipartisan issue in California
Republican Marie Waldron and Democrat Scott Wiener may seem to have little in common. But they have formed an unlikely partnership on an unusual issue: legalizing psychedelic drugs to treat mental illness. Continue reading…
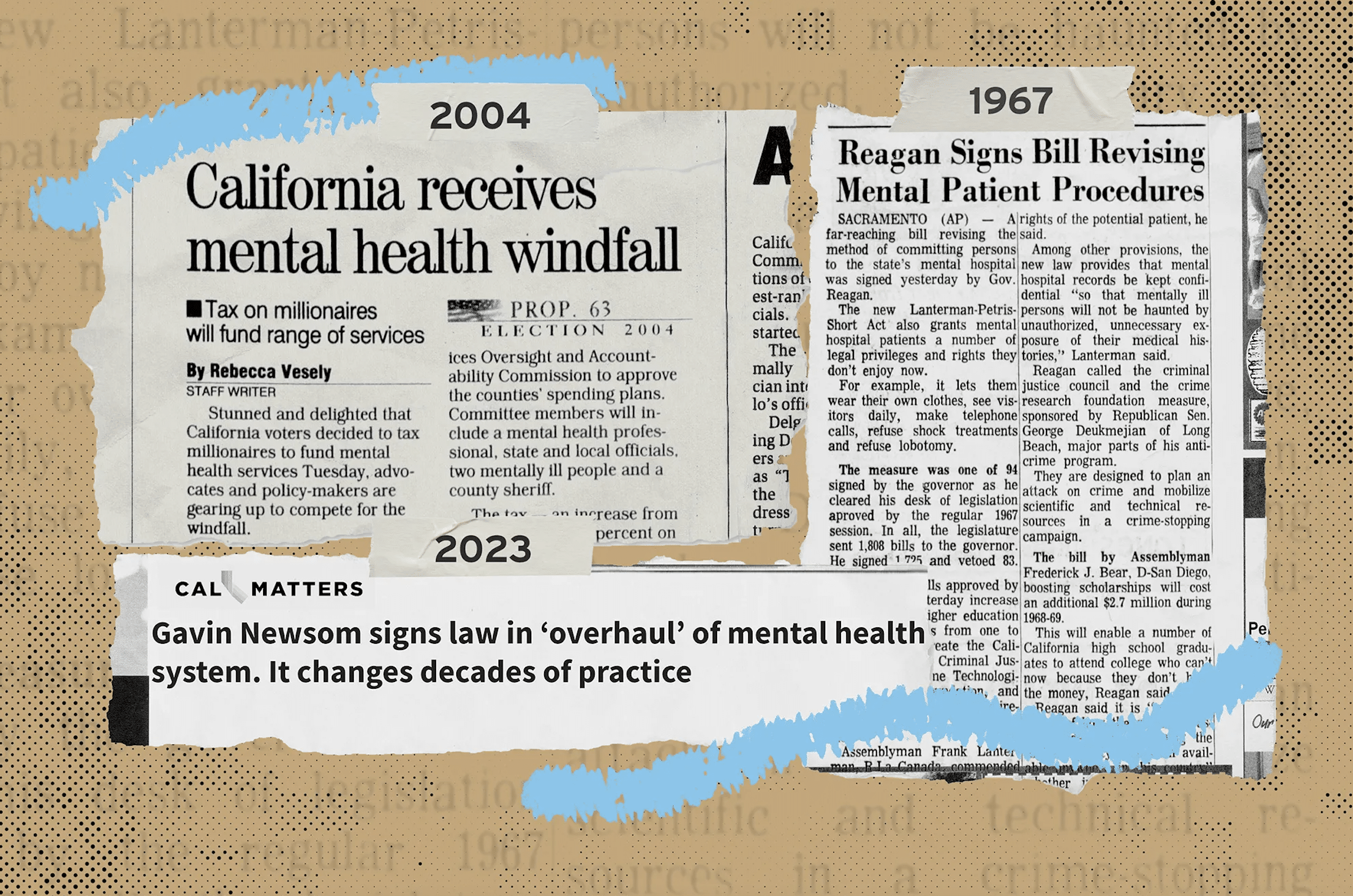
California Voters Will Decide on Newsom’s Mental Health Overhaul. How Did We Get Here?
Proposition 1, a March ballot measure in California, is the latest state proposal that aims to make major changes in mental health policy. Here’s a look at some of the others over the past 75 years. Continue reading…
If you’re not subscribed to MindSite News Daily, click here to sign up.
Support our mission to report on the workings and failings of the
mental health system in America and create a sense of national urgency to transform it.
For more frequent updates, follow us on Facebook, Twitter and Instagram:
The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.
Copyright © 2021 MindSite News, All rights reserved.
You are receiving this email because you signed up at our website. Thank you for reading MindSite News.
mindsitenews.org

Mental health can't wait.
America is in a mental health crisis — but too often, the media overlooks this urgent issue. MindSite News is different. We’re the only national newsroom dedicated exclusively to mental health journalism, exposing systemic failures and spotlighting lifesaving solutions. And as a nonprofit, we depend on reader support to stay independent and focused on the truth.
It takes less than one minute to make a difference. No amount is too small.
The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.