RFK and Trump’s Real Mental Health Agenda: One Disturbing Take
Trump and RFK Jr. are weaponizing anger at the failures of mental health care to gut services and abandon those in need, an analyst writes.

Tuesday, March 4, 2025
By Don Sapatkin

Good Tuesday morning! Today’s Daily may be my newsiest ever: We start with an essay on Trump and Robert F. Kennedy Jr.’s effort to weaponize legitimate anger at the failures of current psychiatric care to gut public services, abandon poor and disabled people, and expand the police state.
Plus: Fountain House Hollywood comes through in a time of crisis. A worrisome global gap has opened between the mental well-being of older vs. younger adults. Psychiatrist Alvin F. Poussaint, a leader on Black mental health, dies at 90. A guide to mental health care for Muslims observing Ramadan. The FDA eases access to the schizophrenia drug clozapine. And desperate French farmers are at their wits’ end.
But first: “How I went from psychedelic facilitator to ketamine addiction in 2 months.” Alison Crosthwait shares and reflects, in her Substack newsletter, Eros for Life.
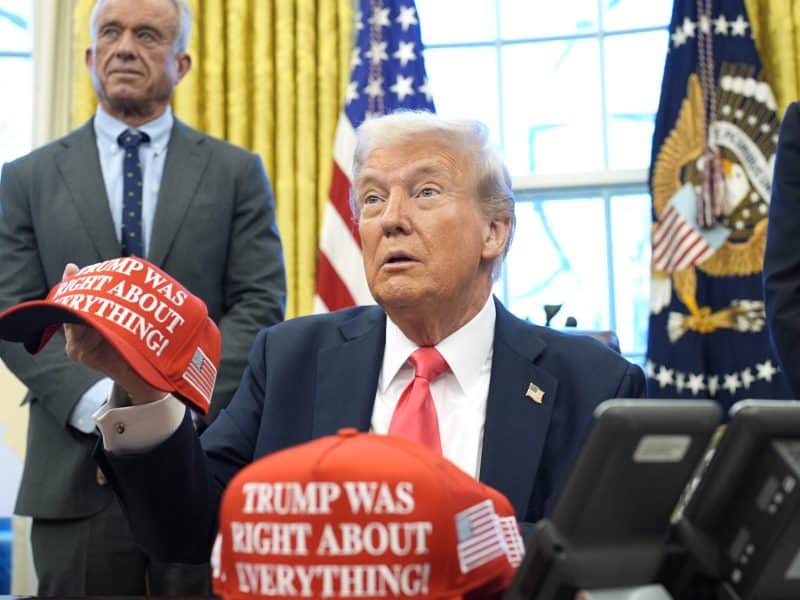
Trump and Kennedy’s real agenda on mental health, according to a psychiatry resident
I just read an analysis in The New Republic by Eric Reinhart, MD, a leftwing psychiatry resident and political anthropologist about how Robert F. Kennedy Jr. and the “Make America Healthy Again” commission that President Trump assigned him to lead will together end mental health care as we know it. I feel like I’ve just taken a high-level graduate course, as opposed to the pre-kindergarten decrees on how to improve mental health treatment through disruption that are spewing from the Trump administration.
Reinhart writes that Kennedy, the new health and human services secretary, is “weaponizing legitimate anger at the failures of psychiatry in order to gut public services, abandon poor and disabled people, and expand the police state.” That’s the subhead on his article. The article itself is more academic – and damning.
Reinhard argues that policies being pursued by Kennedy signal his intention to “radically reshape the nation’s mental health policy” in service of what purports to be a progressive agenda: reversing the over-medicalization of mental and social distress and “challeng(ing) psychiatry’s overreliance on pharmaceuticals, in place of addressing the root social and economic causes underlying much of the human suffering known today as mental illness.”
A longstanding critique of progressives, Reinhard notes, is that “psychiatric diagnoses often obscure the structural causes of suffering – poverty, social isolation, racism, homelessness, and exploitative labor conditions – by reducing them to ‘brain diseases.” Transforming social problems into medical diagnoses feeds pharmaceutical profits and pathologizes oppressed groups. The left’s solution is to demand investments in public systems for nonmedical social care that are sufficient enough to prevent much of the current need for psychiatrists and psychiatric drugs.
Trump and Kennedy, on the other hand, would respond to the same reality by seeking to destroy those systems altogether, plotting major cuts to Medicaid, food stamps, and a gazillion other essential programs that Reinhart contends would leave those in the greatest need with nothing at all. The Trump administration is quickly turning the MAHA agenda “into a eugenics campaign in the guise of reform,” he writes.
“This is not a debate about psychiatry,” Reinhart concludes. “We are in a fight over whether we will, as a society, choose solidarity or abandonment and whether we will meet suffering with care or cruelty.”
We may learn more tonight. Trump’s State of the Union address begins at 9 p.m. Eastern Standard Time.


Fountain House Hollywood’s first big test: recovery after the Los Angeles fires
As the Los Angeles fire raced from Runyon Canyon to Sunset Boulevard in early January, Hope Dixon could see the flames and smoke from the balcony of the Hollywood home where she was sleeping on a friend’s couch. She was already in survival mode when the fires hit – struggling with depression and homelessness after losing her job at a Hollywood production company a year ago.
As her eyes were burned from the smoke, her phone rang – a call from a fellow member of Fountain House, the mental health community and “clubhouse” that she had become a part of, checking in on her to make sure she was OK. “I was so shocked that they actually thought about me,” she told Eliza Partika for a story in MindSite News. “It made me feel really big in the world.”
Just eight months old, Fountain House Hollywood is a mutual support and healing community run by and for people with serious mental illness, with resources provided by the clubhouse. The novel concept first turned into a bricks-and-mortar location in 1940s New York, and now its Hollywood affiliate was playing a vital role supporting its 51 members, who were scattered around Hollywood when the evacuation order came.
In the midst of uncertainty after the fire, Dixon has started a new chapter in her life. Fountain House pushed her to keep believing in herself. “So that’s what I want to do,” she told Partika. “I want to keep growing.”
Across the globe, younger adults are struggling. Older adults are doing better. The combination makes for a perilous future

The mental health and well-being of young people plummeted during the pandemic and have improved only slightly since. For the most part, older adults are OK – and have been all along, based on surveys that began just before the pandemic hit. But in the U.S. and around the world, an average 41% of people aged 18 to 34 continue to experience “functionally debilitating distress,” according to the latest survey from the Global Mind Project.
On functions like planning, language, focus, social interaction, self-control and impulsivity, younger adults are scoring four to five times worse than their elders.
The report comes from Sapien Labs, a research nonprofit that studies how the changing environment and technology affects brain function. Its main analyses are based on more than 1 million responses to the 2023 and 2024 surveys from people in around 80 countries.
The most disturbing findings concern what the report calls “functionally significant problems or challenges” including confused or slowed thinking and physical health problems. On these items, younger adults scored much worse than older adults, with each generation in poorer shape than the last. The findings show the connection between mind and body, the report says, as mental health problems compromise health and immune function.
Perhaps the most interesting finding is that a nation’s greater wealth and economic prosperity don’t equate to better mental health and well-being – especially among young adults, who fared substantially better in some less-developed regions, especially sub-Saharan Africa. Nigeria had the highest score in average mental well-being among 18- to 34-year-olds, followed by other countries in Africa and Central America. Germany, Belgium, the U.S., Canada, Mexico, China and other more developed countries came out much lower, and the U.K. and New Zealand were lower still.
Why the better results in poorer, less-developed countries? It may come down to factors like stronger social, family and community connections, lower consumption of ultra-processed foods, and slower broadband speeds that limit excessive smartphone use, Jennifer Newson, Global Mind’s lead scientist for mental and cognitive health, told MindSite News in an email.
The overall picture is that for young people, especially in wealthy countries, life is getting more difficult. An unrelated working paper commissioned by the United Nations (covering the U.S., U.K., Ireland, Australia, Canada and New Zealand) suggests that our long-held sense of youth being a joyful time of life is no longer true, and that smart phones (and their social media apps) bear a big part of the blame, along with broadening generational inequality.
Two big caveats: The findings in the Sapien Labs study are limited to the “internet-enabled” population, which can be quite different from the general public, especially in developing countries. And the findings have not been peer-reviewed.
In memoriam: Alvin Poussaint, a giant in psychiatry, saw racism’s impact on Black mental health
Alvin F. Poussaint, 90, died at his home in Massachusetts last week, at a moment that resembles the tumultuous period when he first rose to prominence: the late 1970s, when the energy and optimism of the Civil Rights movement faced white backlash and skepticism about the possibility of Black progress in a white-dominated society.
Before that, he had practiced medicine in Los Angeles, then moved to Mississippi to work on desegregating health care. He joined the 1965 Selma to Montgomery march, carrying with him extra medical supplies because he knew that few white people along the route would offer to help. He went on to play a leading role in debates about Black culture and politics in the 1980s and ’90s through his research on the effects of racism on Black mental health.
Poussaint joined the Harvard Medical School faculty in 1969, the same year that he participated in a protest to compel the American Psychiatric Association to address what he saw as neglect and abuse of Black psychiatrists and the Black community. He remained at Harvard for 50 years, becoming an influential voice on race relations, parenting and a range of social issues, while also treating adults and children in private practice.
He was a prolific author. In “Why Blacks Kill Blacks” (1972) and “Black Child Care” (1975), he walked a line between those on the left who blamed persistent racism for the African-American community’s mental health woes and those on the right who said that, in the post-civil rights era, it was up to Black people to take responsibility for their own lives. He told the New York Times in a 2007 interview that he believed many Black men have “a father hunger” and grieve their missing dads in a way that eventually turns to anger: “Why aren’t you with me? Why don’t you care about me?” (A Times obituary last week offered an in-depth story on his life and legacy.)
Poussaint’s charisma and comfort in the public eye made him a force in Black politics and culture, allowing him to make his case to millions. He co-chaired the Rev. Jesse Jackson’s 1984 presidential campaign and was reportedly the model for Dr. Cliff Huxtable on “The Cosby Show,” though he repeatedly denied this. But as a consultant to the show, which ran from 1984 to 1992, he read scripts and sent notes about how to avoid stereotypes or deepen story lines. (This was long before Bill Cosby was accused by more than 50 women of sexual assault and misconduct.)
In 2000, he wrote Lay My Burden Down: Suicide and the Mental Health Crisis Among African-Americans with journalist Amy Alexander, then toured the country with Cosby, interviewing Black men and families. Poussaint and Cosby co-wrote Come On, People: On the Path from Victims to Victors in 2007. By this time, Poussaint was speaking to a new generation of Black Americans, and some found his message simplistic. He also was criticized for arguing that racism was partly a mental disorder, as he did to the APA in a 1999 op-ed for the Times.
The seventh of eight children born to Haitian parents in East Harlem, Poussaint traced his interest in doctoring to a childhood bout of rheumatic fever that left him hospitalized for months, as well as his mother’s death from cervical cancer when he was in high school, according to an obituary posted by Harvard Medical School, which noted that Poussaint was the only Black student in his Cornell University Medical College class in 1960.
The psychiatrist recalled his time in the 1960s South as harrowing. Police officers repeatedly called him “boy,” and threatened to arrest him when he insisted on “Dr.” Those years working with the Civil Rights movement, he told the Boston Globe decades later, made him skeptical of the notion that the United States could overcome its legacy of deep-rooted racism. But he never stopped challenging Black Americans to stand up to systemic bigotry.
In other news…
Ramadan introduces unique mental health challenges, Ankita Guchait, a mental health practitioner who works with refugees in London, writes in a Psychology Today blog post. The period of fasting, prayer, and spiritual reflection is observed by nearly 2 billion Muslims worldwide, this year from Feb. 28 to March 30. Sleep deprivation, medication adjustments, mood fluctuations, and increased social and religious obligations can impact mental well-being, especially for individuals with pre-existing conditions and the histories of trauma often experienced by refugees. In this useful guide, Guchait discusses these challenges and offers suggestions to mental health providers on how to support Muslim patients during the holy month.
Employees are reluctant to discuss their mental health with management, fearing they will be stigmatized or judged, according to a National Alliance on Mental Illness poll of workers and managers at companies with more than 100 staffers. NAMI’s national survey of 2,376 workers age 18 and over was conducted by Ipsos in late January. Among the findings: 26% of respondents said they didn’t know whether their employer offers mental healthcare benefits, an employee assistance program, flexible work arrangements, or sick days for mental health, although more than 80% said these benefits are or would be important to creating a positive workplace culture.
The FDA is expanding access to the schizophrenia drug clozapine, the New York Times reports. Many physicians consider the generic antipsychotic to be the most effective treatment available for the devastating illness, and research shows that it reduces suicidal behavior. It’s the only drug approved for treatment-resistant schizophrenia. But a rare and sometimes life-threatening side effect called neutropenia prompted the agency, in 2015, to impose monitoring obligations on prescribers and patients. The intention is to mitigate risk, but physicians have said it leads to gross underuse of the drug. After lobbying from physicians and testimony from tearful patients, the FDA announced last week that the blood tests before and after prescriptions were filled are “no longer necessary.”
A mental health crisis is “pushing French farmers to a breaking point,” the news organization France24 reports, in a comprehensive look at the issue. France is the European Union’s largest agricultural producer, and its many farming families are struggling amid low sale prices, a higher cost of living, little to no time off, mounting debts and dizzying amounts of paperwork. It’s taking an irreversible toll – farmers die by suicide 43% more than the general population, roughly one every two days. You may recall the mass protests by enraged farmers around this time last year, when convoys of tractors blocked roads in southwest France in a show of force that spread across the entire country. American farmers’ mental health is suffering too, with states and organizations sponsoring crisis hotlines specifically aimed at preventing suicides among agricultural workers.
If you or someone you know is in crisis or experiencing suicidal thoughts, call or text 988 to reach the 988 Suicide & Crisis Lifeline and connect in English or Spanish. If you’re a veteran press 1. If you’re deaf or hard of hearing dial 711, then 988. Services are free and available 24/7.
Recent MindSite News Stories
Homegrown Trips: Veterans Turn to Each Other for PTSD Relief and DIY Psychedelic Treatments
When the sedatives and antidepressants prescribed for PTSD don’t work, some veterans have found peace through psychedelics.
‘We Take Care of Each Other’: Inside the Prison That Could Change Incarceration in America
This prison outside Philadelphia is modeled on prisons in Norway and Sweden that are considered the most humane and effective in the world. “It’s a transformational approach to how we think about prisons,” said a Pennsylvania state legislator.
If you’re not subscribed to MindSite News Daily, click here to sign up.
Support our mission to report on the workings and failings of the
mental health system in America and create a sense of national urgency to transform it.
For more frequent updates, follow us on Facebook, Twitter and Instagram:
The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.
Copyright © 2021 MindSite News, All rights reserved.
You are receiving this email because you signed up at our website. Thank you for reading MindSite News.
mindsitenews.org

Mental health can't wait.
America is in a mental health crisis — but too often, the media overlooks this urgent issue. MindSite News is different. We’re the only national newsroom dedicated exclusively to mental health journalism, exposing systemic failures and spotlighting lifesaving solutions. And as a nonprofit, we depend on reader support to stay independent and focused on the truth.
It takes less than one minute to make a difference. No amount is too small.
The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.









