Mass Layoffs at VA Undermine Vets’ Mental Health
“Destabilizing the VA isn’t saving money: It’s costing veterans priceless care,” says whistleblower about the mass layoffs.


March 25, 2025
By Don Sapatkin

Good Tuesday morning! Recklessness from DOGE accelerates VA tumult. How to prevent overdose deaths in public restrooms. And an influential scientist writes about his recent autism diagnosis.
Plus: Medicaid recipients who could not complete the renewal process report more mental health problems than those who did. A new children’s book follows a Pakistani American middle schooler coping with his father’s schizophrenia. A study finds microdosing LSD is no better than a placebo for ADHD. And Kitty Dukakis will be missed.
Quote of the week: Transitioning as a minor was something that was medically necessary for me to do in order to be not suicidal. – Vivian Jenna Wilson, 20-year-old daughter of Elon Musk, in Teen Vogue.
Bedlam at the VA continues with new threats to patient privacy

For Navy veteran Sandra Fenelon, 33, the transition back to civilian life was a rocky one. She struggled to shake the feeling that she was still “at war.” It took a year of work with a VA psychologist for her to feel safe sharing the troubling experiences from her deployment, things that “people on the outside would never understand.” At a recent therapy session, Fenelson burst into tears, worried that the tumult at the Department of Veterans Affairs will prompt her therapist to leave before she is better. She’s dreading having “to start over with someone else,” she told the New York Times. “How can I relate to a therapist who never worked with veterans?”
In over three dozen interviews, current and recently terminated mental health workers described the chaos at the agency. The VA was already dealing with staffing shortages before Trump and Musk’s layoffs hit. So far 1,900 have been let go, with 80,000 more terminations on the horizon. The turmoil means that some psychiatrists and psychologists are choosing to leave (or retire early) to find other paid work, pushing up wait times and leading veterans to seek care elsewhere.
One particularly troubling change is a mandate that thousands of mental health providers – including many who were hired for fully remote positions – work full time from federal office space. It’s a disconcerting policy reversal for an agency that pioneered virtual health care two decades ago as a way to reach isolated veterans.
Confidentiality seems to be an afterthought. One psychiatrist was stunned to discover that she would have to conduct virtual psychotherapy from one of 13 cubicles, in a large open space that resembled a call center. Earning patients’ trust has sometimes taken months in the privacy of her home office, without potential new fears of being overheard. She feels that the new arrangement violates the ethical and legal requirement of patient privacy. When she raised concerns, a supervisor suggested she purchase privacy screens and a white noise machine. “I’m ready to walk away if it comes to it,” she wrote in a text to her manager that was shared with the Times. “I get it,” the manager replied. “Many of us are ready to walk away.”
The founder and CEO of Whistleblowers of America, who has long advocated for VA whistleblowers who make up 40 percent of all federal employees reporting wrongdoing and filing complaints, can see why. “It’s chaos,” Jacqueline Garrick of the WoA told MindSite News contributor Art Levine. “Destabilizing the VA isn’t saving money: It’s costing veterans priceless care.”
Sensors in public restrooms can prevent drug overdose deaths
Fatal drug overdoses often happen in public bathrooms for three simple reasons: They are located in areas with high foot traffic. They are private. And because users are generally alone, there is no one to spot trouble and administer naloxone to reverse an overdose. Indeed, more than half of U.S. overdose deaths occur when people are using alone.
There’s a relatively simple solution, harm reduction proponents Suhanee Mitragotri and Kevan Shah argue in Health Affairs: Install motion sensor technology to detect when someone enters and exits a restroom, and to monitor the tiny breathing movements of the chest. If the system picks up anything odd, it can alert someone on site who is trained to check the bathroom and, if necessary, respond to an overdose.
One company has installed more than 70 of these sensors in 20 locations across the U.S. and Canada. They have been used in more than 15,000 restroom visits, “successfully detecting 12 overdoses and saving lives,” the authors write. Another company’s device – useful in places like health clinics that see a lot of drug users – alerts staff using a bright flashing light.
The authors note that cost can be a barrier – dual-sensor system costs roughly $2,000 to install plus an annual fee of $500 – and suggest that Congress might appropriate funds, or states’ opioid settlement money could be used to fund installation. But the current climate of cost-cutting, not to mention opposition to harm-reduction interventions, makes cash infusions unlikely.
A scientist diagnosed with autism in mid-life explains why rates spiked. (It’s not vaccines.)
When I first read an essay published last week – “I Was Diagnosed With Autism at 53. I Know Why Rates Are Rising” – I skipped over the byline: Holden Thorp, editor in chief of Science, one of the most prestigious journals in the world. That’s likely why it ended up in the New York Times.
Thorp sets out his beef with HHS Secretary Robert F. Kennedy Jr., who, along with RFK’s boss in the White House, has tasked the CDC with researching whether vaccines are behind a seventy fold increase in autism diagnoses since the 1980s. Thorp notes that this question has already been definitively answered: They are not the cause. He suggests the rise is likely explained by a few factors: greater awareness of the condition (thanks in part to the vaccine controversy and the anti-vax movement it spawned), better identification (especially in women and girls, whose symptoms can present differently), and a broader definition that now includes a range of neurodevelopmental conditions under the umbrella of autism spectrum disorder.
The explanations are all familiar, and backed by scientific evidence, but Thorp connects them to his own experience. As a child in the late 1960s, he writes, “I often stared into space, missed social cues and delivered long monologues about my specific interests.” Autism at that time was considered a form of schizophrenia, mostly diagnosed among children who had huge difficulties in daily functioning and needed extensive support. It wasn’t until Thorp was 53 and interviewed by a psychologist at work, that anyone suspected he had what is now called autism spectrum disorder.
The spectrum includes people with and without intellectual disabilities, and diagnoses have mushroomed only in the latter group. Thorp believes that his neurodiversity has made him a better scientist, because his autistic thinking leads him to search for patterns, and adds: “Knowing I’m on the spectrum has improved my life.”
Medicaid restrictions and the mental health harm of losing coverage: Preview of coming attractions?
As the COVID pandemic swept the country and refused to leave, the Biden administration wanted to make sure people kept access to health care. So it issued rules that allowed people enrolled in Medicaid to maintain their enrollment – without having to prove their continued eligibility. The rolls grew. That rule was lifted in early 2023, and roughly 25 million people lost coverage in the months that followed – a period researchers refer to as “the great unwinding.” It also led, according to a fascinating new study, to anxiety and depression among those who couldn’t manage the bureaucratic process.
The return of re-enrollment requirements created conditions for a “natural experiment” – in this case a study that compares the financial security, mental health and functional health (such as hearing, remembering, understanding, or climbing stairs) of former Medicaid enrollees who wanted to renew their coverage, but couldn’t, compared to those who successfully renewed.
Survey respondents who said they wanted to stay in Medicaid but could not complete the renewal process reported more anxiety, frequent worrying, depression, food insecurity, and difficulty seeing, hearing, and remembering compared to participants who were able to complete their renewals, according to findings published in JAMA Health Forum that compared 131,000 current and former Medicaid enrollees. Of all the survey participants who were disenrolled, 13.5% said it was because they couldn’t complete the renewal process (more than 50% said they no longer qualified).
The results offer a preview of what now may be coming in an even more massive way. The sprawling budget blueprint passed by the House last month calls for $880 billion in cuts to federal Medicaid spending, and much of that is to be achieved by imposing new work or study requirements.
Critics say the whole idea of these rules is to create barriers that many people can’t or won’t meet, resulting in their removal from the program. Indeed, previous reporting on requirements like these has found that a big chunk of the savings comes from pushing otherwise-eligible recipients out of the program, because they were unable to indicate their work hours in online-only forms. Although these cuts have a long way to go before becoming law, the study results hint at what could happen if they do.
Most middle-class Americans, for example, don’t think of Medicaid as their benefit, but many also are surprised to discover that their aging middle-class parents will swiftly run out of money if they need skilled nursing care (median annual cost of a semi-private room in a nursing home is $111,325). Unplanned impoverishment is part of why Medicaid is the primary payor for more than 6 in 10 nursing home residents in the U.S. “This is everybody’s coverage,” David C. Grabowski, a professor of health care policy at Harvard Medical School, told the New York Times.
Additional reading: “What Lies Ahead For Medicaid In Budget Reconciliation?” and “Five Reasons Republicans Won’t Cut Medicaid (Much)” (both Health Affairs) and multiple Medicaid explainers posted by the Kaiser Family Foundation.
In other news…
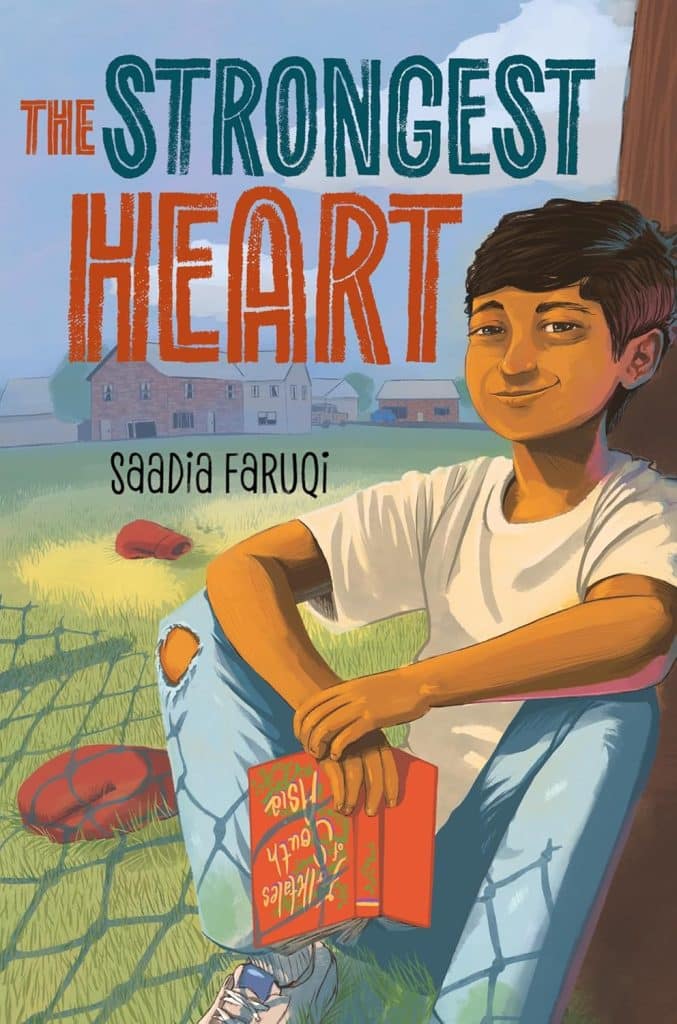
“The Strongest Heart” follows a Pakistani American boy with a schizophrenic father as he struggles to understand his “Abbu.” The just-published book for middle-schoolers is based on author Saadia Faruqi’s own rocky relationship with her father, who she believes had schizophrenia. The Houston-based author spoke with NPR about mental health in Pakistan and what she wishes she could say to her dad if he were alive today.
Microdosing LSD reduced ADHD symptoms – but no more than a placebo, according to a small clinical trial reported by The Microdose newsletter. The findings in JAMA Psychiatry add to concerns about the placebo effect leading to overstated benefits in studies of experimental psychedelic treatments.
Kitty Dukakis, a mental health activist and humanitarian, died at 88. Dukakis – the wife of 1988 Democratic presidential nominee Michael Dukakis, who lost to George H.W. Bush – spoke often about her struggles with addiction and later promoted electroconvulsive therapy as a treatment. She drank heavily following her husband’s defeat, and nearly died from alcohol poisoning on the first anniversary. Antidepressants and treatments including talk therapy didn’t help her much, according to a Washington Post obituary, and she continued to binge drink whatever was available: vanilla extract, mouthwash, aftershave, even nail-polish remover.
Desperate, she turned in 2001 to electroconvulsive therapy (ECT), formerly called shock therapy, which was seen as barbaric, especially after the graphic scenes from 1975’s Oscar-winning “One Flew Over the Cuckoo’s Nest.” For Dukakis, however, the treatments worked so quickly and so well that she called them a “miracle in our lives.” With journalist and author Larry Tye, she wrote the 2006 book “Shock: The Healing Power of Electroconvulsive Therapy.” She died Friday at her home in Brookline, Mass., of complications from dementia.
If you or someone you know is in crisis or experiencing suicidal thoughts, call or text 988 to reach the 988 Suicide & Crisis Lifeline and connect in English or Spanish. If you’re a veteran press 1. If you’re deaf or hard of hearing dial 711, then 988. Services are free and available 24/7.
Recent MindSite News Stories
Inside America’s Mental Health Agency: Mass Firings and Work Stoppages Sap Morale, Impede Mission
The agency tasked with leading the fight to ease the country’s mental health and addiction emergencies is going through an existential crisis. About 100 of its 900 workers have been fired and those that remain are frightened and demoralized. Continue reading…
Opioid Orphans: Grandparents Struggle to Raise Children Left Behind
Despite billions set aside in settlement funds, very little goes to relatives raising bereaved children. Continue reading…
COVID Stole a Parent from Over 200,000 Children. Indian Country Lost the Most
COVID was not an equal-opportunity destroyer. American Indian and Alaska Native children were orphaned at three times the rate of white children, and Black children at double the rate. Without support, children who lose a parent or caregiver are at higher risk of long-term mental health problems.
If you’re not subscribed to MindSite News Daily, click here to sign up.
Support our mission to report on the workings and failings of the
mental health system in America and create a sense of national urgency to transform it.
For more frequent updates, follow us on Facebook, Twitter and Instagram:
The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.
Copyright © 2021 MindSite News, All rights reserved.
You are receiving this email because you signed up at our website. Thank you for reading MindSite News.
mindsitenews.org

The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.










