‘Dementia’ Symptoms Linked to Cirrhosis Are Likely Reversible
What appear to be dementia symptoms in these cases are nearly always reversible with treatment – if they’re linked to undiagnosed liver disease. And more.


February 6, 2024
By Courtney Wise

Greetings, MindSite News Readers! A new study finds that in some cases, what appear to be dementia symptoms may actually be a sign of a treatable condition triggered by undiagnosed liver disease. And today’s top headlines offer some hope in the areas of addiction treatment: The Biden Administration has drafted new rules that will make methadone more accessible to people battling opioid addiction.
Plus, some “anti-crime” laws discriminate against people with mental illness. The work of caregiver spouses doesn’t end when their loved one enters a nursing home. Tips on easing your anxiety over declining social invitations when you really just need to say no. And how Taylor Swift and other Grammy winners have worked the language of psychiatry into their songs.
Study finds up to one in 10 dementia patients may have undiagnosed cirrhosis. If so, their ‘dementia’ symptoms are usually reversible with treatment.
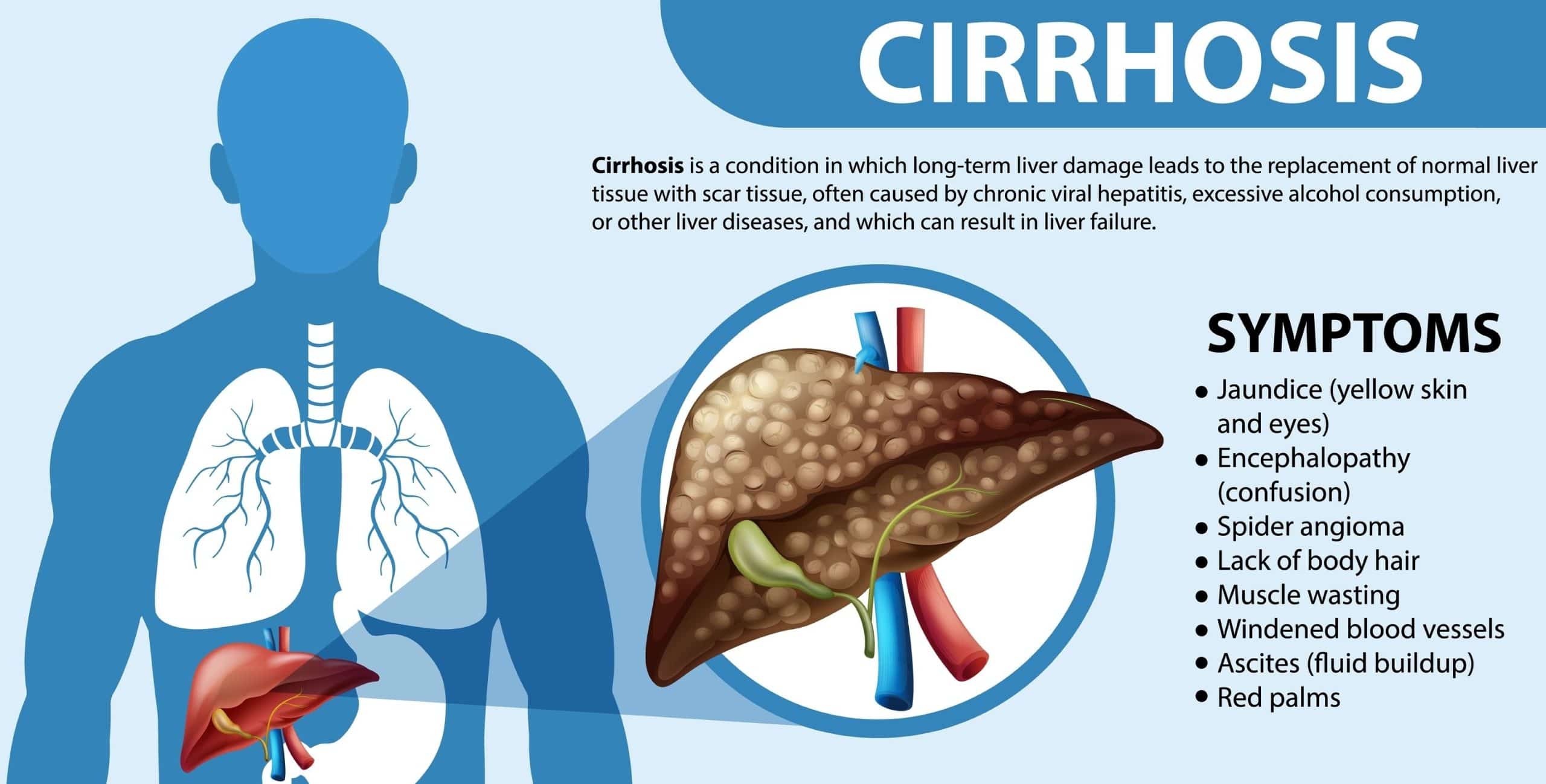
Stunning new research offers hope for a cure in upwards of 10 percent of dementia patients, reports STAT News. That’s based on a study published last week in JAMA Network Open that suggests undiagnosed cirrhosis may cause neurological problems that can be reversed with treatment of the liver disease. The condition, which scars the liver, can be caused by either viruses or disease, including alcohol dependence.
For the study, physicians with Veterans Affairs (VA) analyzed the medical records of 177,000 veterans who were diagnosed with dementia in at least two VA clinics but had never been diagnosed with cirrhosis of the liver. Patients were seen between 2009 and 2019. They sought to find evidence of liver scarring, called fibrosis, and calculated the likelihood of the scarring being caused by cirrhosis using an established formula called the Fibrosis-4 score (FIB-4). They discovered that some 10% of patients had a high enough FIB-4 score to indicate potentially serious liver disease.
What’s that got to do with dementia? Roughly half of people with cirrhosis develop a disorder called hepatic encephalopathy. This occurs when the liver stops clearing toxins from the blood, letting wastes like ammonia accumulate and travel to the brain. The waste then poisons the brain, triggering the negative changes to cognition, motor skills, sleep and mood that are seen in dementia. However, when hepatic encephalopathy is treated with either antibiotics or lactulose to reduce the toxins in the blood or flush them out through the colon, dementia symptoms usually go away. “If a portion of their symptoms is caused by hepatic encephalopathy, which is way easier to treat than dementia, then I think we need to look at that,” said the study’s lead author Jasmohan Bajaj. The trouble is, dementia is hard to distinguish from hepatic encephalopathy, especially in a 15-minute doctor’s appointment. It has to be diagnosed with lab tests.
Liver disease is also hard to catch when first developing, reports STAT. It advances slowly yet steadily over time, becoming evident once severe and/or irreversible damage has been done. Primary care providers tend not to check for it as an issue, unless patients have clear risk factors, such an active alcohol use disorder or a hepatitis B or C infection. Issues like diabetes and obesity are lesser known risk factors for cirrhosis. “It’s not a condition that hurts. Patients don’t come in asking to be screened for cirrhosis,” said Lauren Beste, deputy chief of the general medicine service at the VA Puget Sound Healthcare System. “It’s easy to see why it could be overlooked, but it’s just such an important and lifesaving diagnosis to make early.”
Beste added the FIB-4 score could be used as a screening tool for cirrhosis – but it cannot be used to make a diagnosis. Rather, “it’s a pointer that you need to look harder and rule cirrhosis out” when dealing with dementia symptoms, she said.
Biden Administration expands access to methadone to combat opioid addiction and overdose
Drug overdose deaths have reached an all time high, topping 112,000 last year according to data from the Centers for Disease Control. Most are attributed to the opioid epidemic, which is now turbocharged by fentanyl. Still, two of the most effective treatments for opioid use disorder – methadone (see above) and buprenorphine – remain underutilized. Despite being shown to reduce opioid deaths and relapses by nearly 60 percent, the drugs are rarely prescribed due to strict federal regulations. With supporting data from the National Institute on Drug Abuse, NPR reports that just one in five people experiencing opioid addiction gain access to the medications.
But late last week, the Biden Administration announced new rules intended to widen access to methadone for more people. The changes are slated to take effect this summer. “The easier we make it for people to access the treatments they need, the more lives we can save,” said Health and Human Services Deputy Secretary Andrea Palm.
Under the current rules, methadone is only available through the roughly 2,000 federally-approved opioid treatment programs (OTPs). Primary care physicians are not allowed to write prescriptions for patients and starting doses are fixed, rather than personalized. Moreover, people have to live with opioid addiction for a minimum of one year before receiving the medication.
When the revised rules take effect, methadone will still only be accessible through opioid treatment programs, but patients will have access to more take-home doses, more frequent care after a telehealth consultation, and nurse practitioners and physician assistants employed by OTPs will be allowed to order methadone. In addition, the time required for people to live with opioid addiction before being prescribed methadone will be trimmed to six months.
The news has been met mostly with praise, but legislators and addiction policy experts say the changes aren’t big enough. They’re critical of restricting the authority to dispense methadone to providers at OTPs, rather than also including primary care physicians and local pharmacies. “Ultimately, tethering methadone exclusively to opioid treatment programs is less about access, or health and safety, but about control, and for many investors in those programs, it is about profit,” said Sen. Edward Markey (D-Massachusetts). “The longer we leave this antiquated system in place, the more lives we lose.”
Minnesota city discriminated against people with mental health disabilities: DOJ
Using “anti-crime” laws to discriminate against people with mental health disabilities (and landlords who rent to them): The US Department of Justice found that the city of Anoka, Minnesota enacted a ‘crime-free’ ordinance in a way that made it difficult for renters with mental health issues to secure or maintain housing. Claiming a desire to deter crime and prevent public nuisances, CBS News reports that Anoka officials issued weekly reports to landlords that included personal medical information of tenants who had multiple emergency calls to their homes.
“The department found that people with mental health disabilities and their families or service providers refrained from calling for help to avoid risking their current housing or future housing prospects,” the Department of Justice reported. “This scheme is cloaked as a public safety measure but in reality it callously targets people with disabilities and their loved ones by penalizing them simply for reaching out for emergency assistance in times of need.”
Among other things, the DOJ found, the ordinance allowed the city to suspend a landlord’s rental license if police respond to four or more “nuisance” calls to their property within 12 months and/or if the landlord refuses to evict the renters in question. They could be fined for four calls or less. The Department of Justice has ordered the city to change its policies, hire an ADA coordinator and train its staff – a move welcomed by mental health advocates. First responders wouldn’t punish someone for having to respond to multiple heart-related issues, said Sue Abderholden, executive director of the National Alliance on Mental Illness Minnesota chapter. “Why would we do it when somebody has a mental health issue?”
Caregiving stress doesn’t end for spouses when partners enter a nursing home
The choice to move a loved one into a long-term care facility comes when necessary – but not easily. Though spouses tend to make the tough decision once they’re no longer able to care for their partners at home, the relief that comes from no longer having to provide around-the-clock care is often replaced by anxiety and guilt. Joseph Drolet, 79, told the New York Times that the stress of providing 24-hour care for his wife who was diagnosed with Alzheimer’s went away after he placed her in a nearby memory care facility, relieving him of the fear of what would happen to her if he died or became disabled. But, those concerns were quickly replaced with new worries. He didn’t believe she was as content or well-cared for as she was when at home with him. There is also the pain of an empty house, “where everywhere I look is the reminder of her absence,” he said, weeping.
“Too often, institutionalization is thought of as the end of family caregiving. It’s not,” said gerontologist Joseph Gaugler. In fact, shouldering the new tasks of overseeing care, advocating on behalf of the resident and monitoring the staff means that “in some ways, there’s a chance of substituting one set of challenges for another.”
Studies show that spousal caregivers tend to be more likely to continue providing daily care, even after their loved one moves to a facility. Social psychologist Richard Schulz found that almost half of spouses visit their partners every day, compared to one quarter of children, siblings, and other caregivers. When present, family members help staffers with personal care like feeding, grooming, moving around, and participating in activities.
Support groups and other programs designed to educate and provide resources to family caregivers help reduce some of the mental distress caregivers experience. Therapy and antidepressants are useful, too. Drolet employs each of the aforementioned tools to help him as his wife moves through hospice care. I’m “dreading visits while loving them,” he said. “There are no happy tomorrows in this situation.”
In other news…
Days ago, the Grammys hosted their 66th annual award show. Considering the ways in which the language of psychiatry is showing up in popular music, Ellen Barry of the New York Times reached out to mental health clinicians to learn how various Grammy winners’ work shows up in their offices. A therapist in Chattanooga, Tennessee, told the Times some of his male clients who had trouble opening up called on Taylor Swift lyrics to express their pain. “’When they’re talking about it in a song, it arms them with some words they don’t have,’ he said. Her lyrics exploring damage left after breakups, he said, have ‘made them rethink how they do relationships.’”
Declining social invitations triggers major anxiety in some people. People fear hurting their friends or losing out on other opportunities in professional situations. But as my cousin used to say, “the worry is worse than the wear.” In other words, saying no is healthier than stressing about the “what ifs” that might follow. Plus, researchers told the Washington Post that people overestimate the negative implications of declining an invite. They also offered some tips on how to say no to the next outing you just don’t want to attend.
If you or someone you know is in crisis or experiencing suicidal thoughts, call or text 988 to reach the 988 Suicide & Crisis Lifeline and connect in English or Spanish. If you’re a veteran press 1. If you’re deaf or hard of hearing dial 711, then 988. Services are free and available 24/7.
Recent MindSite News Stories
The Night Parade: A genre-bending memoir that helps reshape the cultural narrative on bipolar illness and grief
Jami Nakamura Lin has written a rich, exquisitely illustrated memoir that expands the cultural narrative on mental illness and grief. Continue reading…
A Former Hotline Counselor ‘Hands the Mic’ to Call-takers to Amplify Their Voices
The author of a survey of crisis hotline counselors talks about his experiences and why he wanted to tap into the wisdom of the people who answer calls to 988. Continue reading…
988-Hotline Counselors Air Concerns About Lack of Training, Rushed Calls
A newly released report, based on responses from 47 crisis counselors, explored variations in their training and work experiences. The first-of-its-kind survey raised raised the voices of 988’s workforce and surfaced some interesting snapshots.
If you’re not subscribed to MindSite News Daily, click here to sign up.
Support our mission to report on the workings and failings of the
mental health system in America and create a sense of national urgency to transform it.
For more frequent updates, follow us on Facebook, Twitter and Instagram:
The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.
Copyright © 2021 MindSite News, All rights reserved.
You are receiving this email because you signed up at our website. Thank you for reading MindSite News.
mindsitenews.org

Mental health can't wait.
America is in a mental health crisis — but too often, the media overlooks this urgent issue. MindSite News is different. We’re the only national newsroom dedicated exclusively to mental health journalism, exposing systemic failures and spotlighting lifesaving solutions. And as a nonprofit, we depend on reader support to stay independent and focused on the truth.
It takes less than one minute to make a difference. No amount is too small.
The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.