Suicide Rising Among Women Veterans
A report shows a sharp rise in suicides by female veterans, and inadequate VA services to prevent them. A new study in twins shows the impact of trauma in childhood while controlling for genetic factors.

Monday, March 11, 2024
By Don Sapatkin

Good Monday Morning! Lots of news for you today: A report shows a sharp rise in suicides by female veterans, and inadequate VA services to prevent them. A new study in twins shows the impact of trauma in childhood while controlling for genetic factors.
Plus, the ripple effect of overdose deaths on those left behind constitute an “overlooked emergency.” More workers than ever are taking mental health leaves of absence. And a former weapons trainer’s years of exposure to grenade blasts left massive brain damage that may have led to him becoming a mass shooter.
Suicide among women veterans is spiking. Many feel the VA is failing them, a new report says
Carmen McGinnis enlisted in the Marines on Sept. 11, 2001, the day after she turned 17. She eventually deployed to Afghanistan, but her scariest experiences were repeated sexual harassment and a violent sexual assault.
The military offered little in the way of mental health care, McGinnis said, and she overexercised, experienced insomnia and lost an unhealthy amount of weight before leaving the military in 2008.
As a civilian, she grappled with undiagnosed PTSD related to the assault and didn’t care whether she lived. When she told her VA primary care provider she was drinking too much, he said it wasn’t a problem since she was drinking red wine, which was good for her. “It just totally broke my spirit of asking for help or doing anything,” McGinnis said.
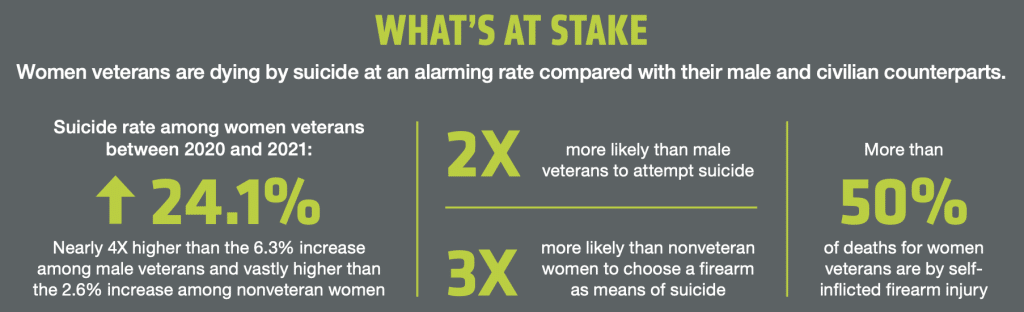
A new report from Disabled American Veterans (DAV) looked at these issues. It notes that women now make up 10% of American veterans and that one in three say they’ve experienced military sexual trauma – which includes both harassment and assault and raises the risk of substance abuse and suicide. Other key findings: Female veterans’ suicide rate jumped 24% from 2020 to 2021, a much steeper rise than among male veterans and nonveteran women. More than half of women veterans’ deaths are by self-inflicted gun injury. And for female veterans, going through menopause – the period of greatest suicide risk among women generally – can be compounded by PTSD, depression substance use disorders and past sexual trauma, creating what Air Force veteran Maria Luque calls “a perfect storm.”
While VA’s mental health outreach to women has improved in recent years, the agency too often overlooks women’s needs when crafting mental health programs and relies on male-focused messaging, the DAV report says. Suicide prevention efforts, for example, don’t address sexual trauma or perinatal issues, both of which increase the risk of suicide among female vets. “The lack of recognition for women’s service, isolation after separation from military service, poor social support and unique risk factors all contribute to the challenges and barriers that many ill and injured women veterans face as they transition from service members to civilians,” the report states.
The report details personal stories of female veterans and the many ways the system fails them. It also makes more than 50 recommendations, including these:
•Make military sexual trauma a central pillar of suicide prevention efforts and ensure that veterans are effectively screened for it.
•Create a three-digit number, a la 988, with a veteran option, for the National Domestic Violence Hotline (800-799-7233).
•Revise the VA model for predicting suicidality to incorporate risk factors weighted for women veterans.
•Convene experts in menopausal women’s health to explore a research agenda on the related threads of menopause and suicide.
Childhood trauma boosts odds of adult mental health problems even after controlling for genetics, a study of twins finds
Lots of research has shown that the impact of childhood trauma can carry into adulthood, boosting the lifelong risk of physical and mental health conditions. But since adverse childhood experiences or ACEs often cluster in families, it can be hard to tease out the effect of genetics from that of trauma.
Now a new study has used a classic technique by following every pair of twins born in Sweden between 1959 and 1998 – more than 25,000 adult twins in all – to separate these two factors.
The study, published in JAMA Psychiatry, considered ACEs such as family violence, emotional abuse or neglect, physical or sexual abuse, rape and neglect. Each ACE experienced as a child by those in the study boosted by 52% their chances of being diagnosed with a psychiatric condition as an adult. The more ACEs, the greater the risk: Among those who reported three or more adverse experiences, nearly a quarter had a psychiatric diagnosis in adulthood.
The researchers also analyzed a subset of “discordant” pairs in which only one of the twins reported trauma. The effect was less, but still significant: A twin who reported maltreatment was 20% more likely to have an adult mental illness than their non-traumatized identical twin and 29% more likely than a fraternal twin. The impact was especially pronounced among twins who reported sexual abuse, rape and physical neglect.
“These findings suggest greater influence than I expected,” said identical twin and study co-author Hilda Bjork Danielsdottir, a doctoral candidate at the University of Iceland. Twins may diverge in their experiences of childhood trauma for many reasons, she told the New York Times, noting that in 93% of cases in which a study participant reported a rape, the other twin had not experienced it. Mark Bellis, a public health professor who wasn’t involved with the study, told the Times that by ruling out the role of genetic factors, the findings add to the “irrefutable evidence that it is going to cost us all a lot less if we invest in tackling” abuse and neglect of children now rather than “continuing to pay for the epidemic levels of harm” they cause downstream.
In an unrelated survey, U.K. psychiatrists said abuse and violence against women and girls is the main reason they’re much more likely than s to develop mental health problems, The Guardian reported. The top three contributors to poor female mental health were violence and abuse (named by 59% of participants); relationship issues, often involving coercive behavior (49%); and home and family pressures (48%). “Victims often feel unable to speak openly about such issues, meaning their problems go unnoticed, sometimes for years,” said psychiatrist Catherine Durkin of the Royal College of Psychiatrists, which conducted the survey.
An ‘overlooked emergency’: 1 in 8 adults have been impacted by the overdose deaths of others
Drug overdoses don’t just cut short the life of a person, they also can have a profound effect on friends and family left behind. In a new survey conducted by the RAND Corporation, 42% of respondents – equivalent to 125 million American adults – said they personally knew someone who died of an overdose.
Among them, 19% said they knew two to five people who died of an OD, and 5% knew six or more, perhaps reflecting the high number of fatalities occurring in communities of drug users.
Nearly a third of those who knew an overdose victim said that the death disrupted their lives – the equivalent of more than 40 million people, 13% of the adult population). For 4% of those left behind, the loss had a significant or devastating effect that they still feel. Kerry Nolte, a nurse practitioner who was not involved in the RAND survey, told CNN that she had lost at least six people to overdose that she knew personally.
“Grief from these losses continues to affect me, but it motivates me to continue to do the work of supporting people who use drugs and those that experience trauma,” said Nolte, an associate professor of nursing at the University of New Hampshire. The findings were published in the American Journal of Public Health.
In other news…
An autopsy of mass shooter Robert R. Card II’s brain found shredded connections, blood vessels so battered they could no longer support neurons, and clumps of dead cell debris. These markings of brain injury in an Army Reservist who never saw combat – but was exposed to thousands of grenade blasts as a training instructor – raise huge questions for the military and millions of American veterans, the New York Times reported. Card killed 18 people, then himself, in the deadliest shooting in Maine’s history. He had never deployed to a war zone or played football, activities known to cause traumatic brain injuries. But “brain injury likely played a role” in behavioral changes he exhibited in the months before the October shootings, Ann McGee, a Boston University brain researcher, told the Washington Post.
Mental health leaves of absence from work increased by a third in 2023, continuing a long-term trend, reported ComPsych, a company that bills itself as the world’s largest provider of mental health and absence management services for businesses. The rise has been driven largely by women, who took 69% of the mental health leaves last year – almost two-thirds of them taken by Millennials and Gen X’ers. ComPsych founder and CEO Richard A. Chaifetz pointed to the pressures of managing teams, buying a home for the first time or acclimating to work as a new parent. “HR teams must invest in resources and programming that relates to issues commonly faced by these demographics,” he said.
The City of Los Angeles Fire Department wants to end a 4-year-old pilot program that sends mental health workers on non-emergency calls, saying it didn’t actually free up first responders and hospital emergency rooms, the Los Angeles Times reported. The program sent a van with a psychiatric response team instead of paramedics or EMTs to handle 911 calls involving patients suffering nonviolent mental health crises. A fire department report said the idea was “sound in theory” but not in practice. Fewer than four patients a day met the narrow criteria established for transport by a therapeutic van last year. The City Council will consider the recommendation.
A phone app under development can detect early signs of depression even before the user is aware of it with 75% accuracy, the Politico Future Pulse newsletter reported. Dartmouth College researchers recruited 177 people to answer questions about feeling down, depressed or hopeless while an app captured images of them. The researchers then used artificial intelligence to train the app to correlate self-reports of feeling depressed with facial expressions such as gaze, eye movement, head position and muscle rigidity, as well as ambient elements like dominant colors, lighting, photo location and the number of people in the picture. If someone consistently appeared with a flat expression in a dimly lit room for an extended period, the AI model might infer that the user was depressed. The authors plan to present their findings at the Association of Computing Machinery conference in May.
If you or someone you know is in crisis or experiencing suicidal thoughts, call or text 988 to reach the 988 Suicide & Crisis Lifeline and connect in English or Spanish. If you’re a veteran press 1. If you’re deaf or hard of hearing dial 711, then 988. Services are free and available 24/7.
Recent MindSite News Stories
8 Ways to Deal With the Loss of a Beloved Pet
It’s hard for parents to know what to do when a beloved pet dies — and how to comfort their children. Psychologist Barbara Greenberg has some advice.
Can Prop. 1 Address California’s Trifecta of Mental Health Crises? Voters Are About to Decide
As voters prepare to pass judgment on Proposition 1, MindSite News asked six key players in the state’s constellation of mental health services to weigh in on its likely impact. Will it finally succeed in helping the state address a […]
How psychedelic drug therapy became a rare bipartisan issue in California
Republican Marie Waldron and Democrat Scott Wiener may seem to have little in common. But they have formed an unlikely partnership on an unusual issue: legalizing psychedelic drugs to treat mental illness.
If you’re not subscribed to MindSite News Daily, click here to sign up.
Support our mission to report on the workings and failings of the
mental health system in America and create a sense of national urgency to transform it.
For more frequent updates, follow us on Facebook, Twitter and Instagram:
The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.
Copyright © 2021 MindSite News, All rights reserved.
You are receiving this email because you signed up at our website. Thank you for reading MindSite News.
mindsitenews.org

The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.