An In-Depth Look at New Mental Health Parity Rules
Today’s Daily is devoted entirely to a new set of final federal regulations released last week by the Biden administration that are aimed at forcing health insurers to equitably cover mental health services.


Monday, Sept. 16, 2024
By Don Sapatkin

Happy Monday! Today’s Daily is devoted entirely to a new set of final federal regulations released last week by the Biden administration that are aimed at forcing health insurers to equitably cover mental health services.
So far, the wonky new rules have received little attention from major media outlets even though many policy experts say they represent the most significant effort in more than a decade to expand access to behavioral health treatment.
The new rules add teeth in surprising ways to existing laws that were passed in an effort to require insurers to cover mental health and addiction services on par with what they routinely provide for other medical conditions.
In a statement issued by the White House when the rule was released on Sept. 9, President Biden put it this way: “There’s no reason that breaking your arm should be treated differently than having a mental health condition.”
The regulations lay out rules of the road to guide enforcement of laws passed by Congress over the past couple of decades, especially the Mental Health Parity and Addiction Equity Act of 2008 and some subsequent revisions. While we’ve been hearing for years that these laws would make mental health parity a reality, the reality has been quite different: The gap in coverage between mental health and substance use disorders on the one hand and medical and surgical treatment on the other has been growing in recent years.
The Biden administration and advocates that have been pressing for reform say these new regulations will finally make a real difference: Prior authorization requirements will plummet. Therapists will get raises. Health plans will – get this! – actually be fined if they continue trying to restrict benefits rather than expanding them.
Perhaps the biggest thing the new rules add is greater “required transparency” from health insurers, said Mark Dunn, director of public policy for the National Association of Addiction Treatment Providers. And that, theoretically, should make them more effective.
But a lot could still go wrong. Industry groups are threatening litigation and a recent ruling by a Supreme Court clearly hostile to regulation could defang the new rules. And to the extent they are implemented, they may increase the burden on insurers and boost the cost of premiums.
A brief primer on the new rules
The new final rule applies to nearly all forms of commercial health insurance in the United States, including plans covering more than 175 million Americans that are regulated by three federal agencies. This includes Medicaid managed care plans, which cover more than 75% of Medicaid enrollees in most states.
The mind-bogglingly complicated regulations will be published in the Federal register next Monday, but until then, the Dept. of Labor has provided a fact sheet summarizing the new rules. The National Law Review has a short summary here, and Kaiser Family Foundation has one here.
The first thing you need to know is that the parity law does not require insurers to cover mental health and addiction coverage, but it does require those that offer mental health benefits to refrain from imposing limitations that are stricter than limits placed on medical and surgical offerings. The regulations define two principal types of coverage limitations used by insurers:
• “Quantifiable treatment limitations” (QTLs) are the limits on coverage that can be counted and compared – things like the number of inpatient or outpatient treatment days that a plan will cover. This area may be the 2008 parity law’s biggest success story to date. It took the Obama administration five years to issue final regulations to implement the law, but once it did, insurers moved away from evident violations of QTLs. Today, for example, most plans no longer impose a limit on the number of mental health therapy sessions that is lower than the limit on physical therapy sessions. Similarly, annual and lifetime limits on behavioral health services used to be far lower than for medical coverage – but they are now more similar.
• “Non-quantifiable treatment limitations” (NQTLs) are restrictions that cannot be reduced to numbers – things like requiring prior authorization for a covered treatment; maintaining an adequate number and availability of providers listed as part of an insurers network; the medications included in an insurer’s formulary, and at which tiers. Precisely because they are so hard to measure, these are the areas where insurers had the greatest ability to limit treatment – and have been the law’s biggest failure. For years, neither regulators nor insurers knew exactly how to manage these, and many insurers didn’t bother to try, even though the law required it.
Federal and state regulators have complained that trying to get insurance plans to meet the requirements was like playing whack-a-mole: As soon as one obscure NQTL issue was brought into compliance, health plans would find other ways to get around the requirement. And there was no clear mechanism for enforcing the parity requirements on NQTLs. Today, the new parity rule focuses strongly on these hard-to-measure treatment limitations – and it does so by requiring greater data and transparency.
“Plans have to collect and analyze data on how their practices limit access to mental health and addiction treatment, and compare it to practices for physical health,” said David Lloyd, who has worked on parity issues for years and is now the chief policy officer at Inseparable, an advocacy organization that focuses on policy change to improve access to mental health services.
After collecting and analyzing the comparative data, insurers are supposed to act on their findings and make changes to come into compliance with the law. They also are supposed to report this comparative data annually, and regulators can request it at any time. If regulators find that insurers have imposed coverage limitations that are more onerous for mental health than for medical services, they can order the plan to drop the limitation entirely – a big and costly deal if the limitation applies, for example, to prior authorizations, Lloyd said.
The frustrating hunt for in-network providers
One of the biggest barriers that keeps insured patients from getting the mental health care they need is the extreme difficulty they have finding clinicians who are in an insurer’s provider network – and are actually available to provide service. Many patients wait months to see a psychotherapist, if they can find one at all. In-network providers offering physical health care are rarely so hard to find.
Patients went out of network to see a psychologist for an office visit 10 times more often than they did to see medical or surgical specialists, according to an exhaustive report on network parity published in April by RTI International. The study also examined reimbursement rates, which many clinicians say are so low they have to leave insurance networks and see only self-paying clients in order to make a living. The RTI researchers found that health plans paid medical clinicians 22% more than behavioral health clinicians for office visits and physician assistants 19% more than psychiatrists.
Under the new regulations, it doesn’t matter why a health plan can’t maintain a robust network of behavioral health clinicians – it is required to do so for each category of provider and facility. Creating truly adequate networks is likely to be expensive, and many clinicians who left say it would take a lot to entice them back.
Insurers, not surprisingly, say the new regulation “will be impossible to operationalize, resulting in worse patient outcomes” and will cause “severe unintended consequences that will raise costs and jeopardize patients’ access to safe, effective, and medically necessary mental health support,” according to a joint press release issued by three insurance industry organizations. They said there are other, “proven solutions to increase access to mental health and substance use disorder care,” including expanding the mental health workforce, expanding telehealth, and improving training for primary care providers.
The litigation threat
One group, an association of large, self-insured employers called ERIC, threatened legal action against the new rules. “We will consider all possibilities to prevent further harm to employers offering behavioral health benefits, and the employees and families who count on them – up to and including litigation,” said Melissa Bartlett, ERIC’s senior vice president of health policy.
Arthur C. Evans Jr., CEO and executive vice president of the American Psychological Association, supports the new rule, as do most organizations representing providers. He contends that the failure to cover mental health services means that many patients don’t get needed help – and, as a result, often end up needing more expensive medical treatment.
“If they look at their own data, they will find that what’s driving their health care costs is people with behavioral health conditions” who get sick and have medical complications more frequently than people with only physical health issues, Evans said.
The final parity rule landed at a fraught time in politics and law. Rules like this one normally are hard to repeal if a new party takes control and wants to change course. But the rule’s release so close to Election Day may muddle things. And while expanding access to mental health and addiction treatment has enjoyed bipartisan support, efforts to enforce these new rules may face serious headwinds. The insurance industry’s hostility toward the new rule may peel off support from Republicans and Democrats skeptical of regulation and who may want to curry favor with insurers.
The outlook in the courts has changed as well. In the past, a legal challenge to an administration rule of this kind might have been an uphill battle. But in June, a landmark decision by the Supreme Court’s conservative majority overturned the longstanding Chevron doctrine and removed the deference that had been granted to the expertise of federal agencies in assessing and crafting regulations. The decision is likely to invite insurers to challenge actions by federal regulators.
Administration officials have said they’ve written the new regulations in a way that is consistent with applicable law, and Mark Dunn, from the treatment providers association, hopes they’re right.
“We’re hopeful,” said Dunn. “This gives us more tools than we’ve ever had to implement the law.” Still, he added, “given some of the recent Supreme Court decisions, who knows?”
If you or someone you know is in crisis or experiencing suicidal thoughts, call or text 988 to reach the 988 Suicide & Crisis Lifeline and connect in English or Spanish. If you’re a veteran press 1. If you’re deaf or hard of hearing dial 711, then 988. Services are free and available 24/7.
Recent MindSite News Stories
House, Senate Committees Release Dueling Mental Health Spending Bills
Senate and House committees have put forward two sets of fundings bills for mental health and addiction services. The results won’t be decided until the lame-duck Congress meets after the November elections.
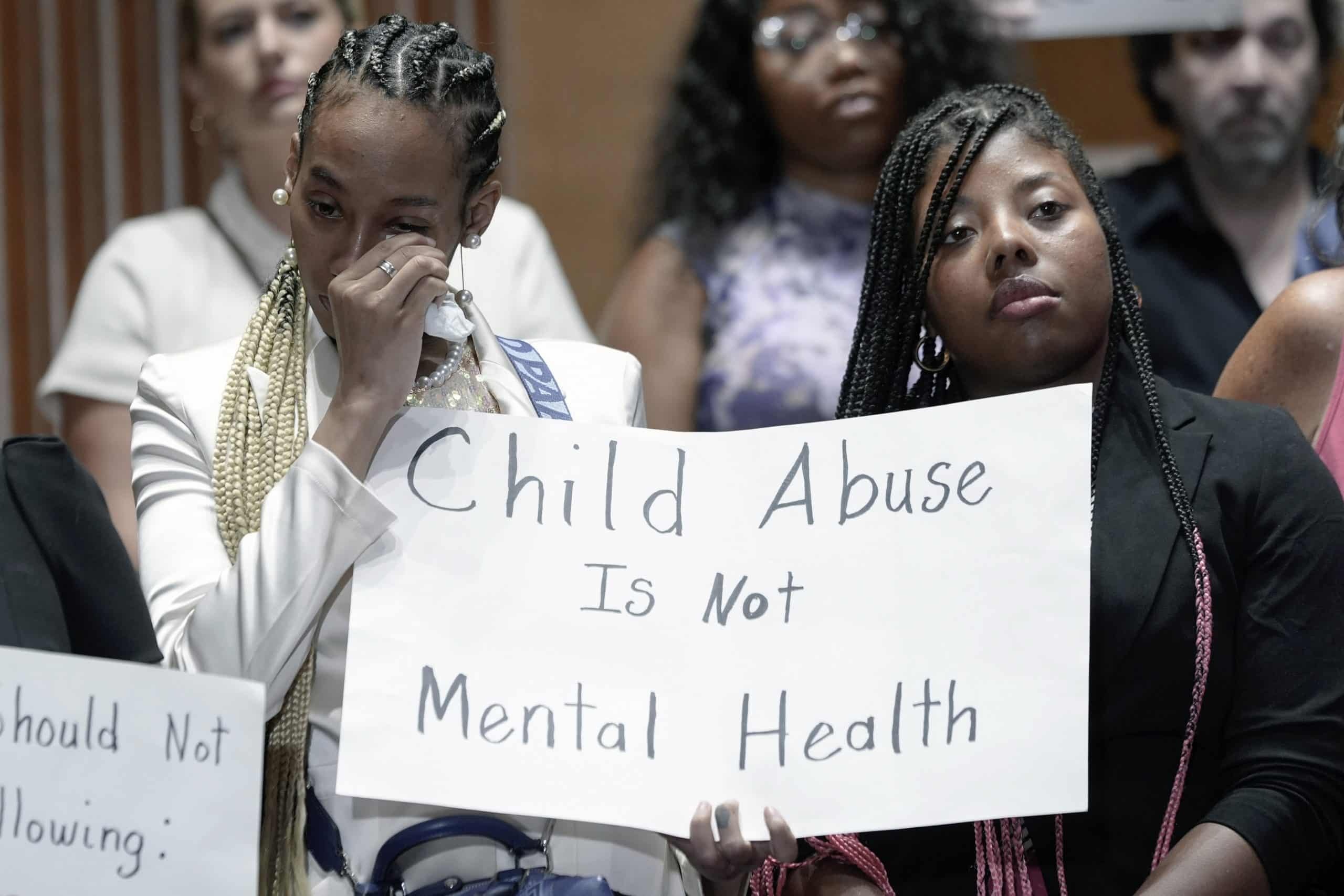
How Paris Hilton and Other Survivors of the Troubled Teen Industry Unleashed a Movement
Meet Five True-Life Avengers Who Are Holding the Troubled Teen Industry Accountable
Troubled Teen Industry Is ‘Taxpayer-Funded Child Abuse,’ Senate Report and Paris Hilton Say. Where Are the Government Regulators?
Physical abuse, rape, and emotional trauma is endemic to psychiatric residential treatment centers for kids and youth nationwide.
If you’re not subscribed to MindSite News Daily, click here to sign up.
Support our mission to report on the workings and failings of the
mental health system in America and create a sense of national urgency to transform it.
For more frequent updates, follow us on Facebook, Twitter and Instagram:
The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.
Copyright © 2021 MindSite News, All rights reserved.
You are receiving this email because you signed up at our website. Thank you for reading MindSite News.
mindsitenews.org

Mental health can't wait.
America is in a mental health crisis — but too often, the media overlooks this urgent issue. MindSite News is different. We’re the only national newsroom dedicated exclusively to mental health journalism, exposing systemic failures and spotlighting lifesaving solutions. And as a nonprofit, we depend on reader support to stay independent and focused on the truth.
It takes less than one minute to make a difference. No amount is too small.
The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.