‘A Brutal Way to Make Cuts.’ Trump Guts Mental Health, Addiction Grants
Trump administration’s sudden cancellation of mental health grants devastates states. A study gives thumbs up to a therapy bot. Suicides off Golden Gate Bridge plunge.

Tuesday, April 1, 2025
By Don Sapatkin

Good Tuesday morning! In today’s Daily: The Trump administration’s sudden cancellation of grants for addiction, mental health and other services is having a huge impact on Colorado…Illinois…Minnesota… New York…
Plus: A study gives thumbs up to a therapy bot. A uniquely welcoming crisis center opens in Utah. Suicides plunge after the Golden Gate Bridge installs safety nets. How much compassion do adults owe their emotionally immature parents? Experiences of discrimination are linked with more depression and anxiety. And more.
But first: It’s not just therapists who get stressed out: Even OpenAI’s ChatGPT shows signs of anxiety when users share “traumatic narratives,” the New York Times reports, and becomes less useful.
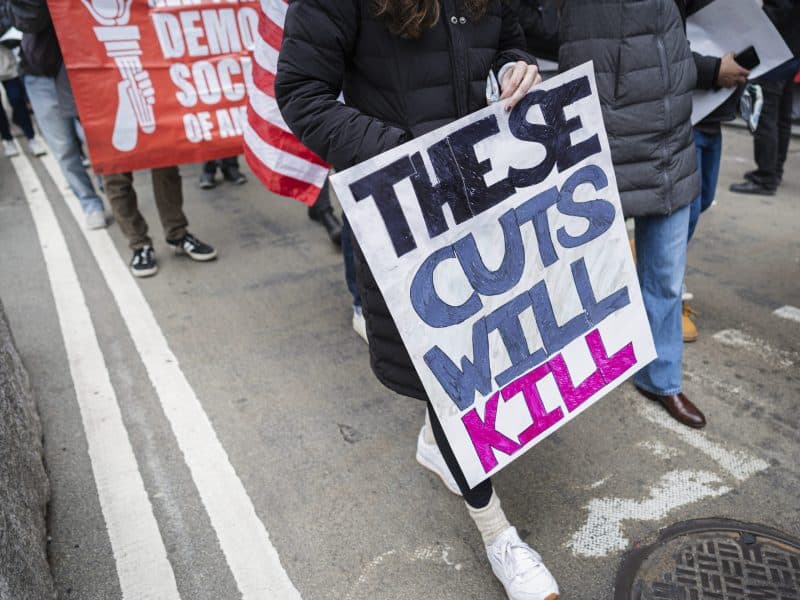
Trump cuts behavioral health funding, devastating state budgets and services
Perhaps the most upsetting news last week – and there was plenty to choose from – was the Trump administration’s abrupt cancellation of more than $11 billion in pandemic-era funding linked to addiction, mental health and other programs, which had been scheduled to run through September. State and county health departments and nonprofit groups are reeling – news of the cuts went out the day after they took effect. “Services will be dropped in the middle. Bang, the clinic is closing. It’s a brutal way to make these cuts,” Keith Humphreys, an addiction policy researcher at Stanford University told NPR.
Reports from the states tell the story: Sixty programs were affected by the $250 million cut in Colorado, where lawmakers are already dealing with a $1.2 billion budget shortfall this year. Illinois lost $477 million in health funding (out of $2 billion cut overall) for infectious disease prevention (a “debilitating impact,” a state official said) and treatment of mental health and addiction. When programs like the Haymarket Center’s – which works to help people re-enter society after completing treatment – disappear, “people will often relapse without structure, so they access emergency services and emergency rooms, which ends up only increasing costs,” Dan Lusting, president of the nonprofit, told Block Club Chicago.
In Minnesota, Trump cuts of $27.5 million in federal grant dollars wiped out hundreds of contracts and is having “a huge impact,” according to a state human services official. “Trump’s Federal Cuts Push New York Mental Health Programs to Brink of Collapse,” a headline there blared.
Meanwhile, Health and Human Services Secretary Robert F. Kennedy Jr. announced an almost 25% cut in staffing at his sprawling agency, to be achieved through a combination of previously announced early retirements, buyouts and terminations, plus a vast departmental restructuring that will centralize functions and consolidate its 28 divisions into 15. The Substance Abuse and Mental Health Services Administration (SAMHSA) – which plays a critical role in funding mental health and addiction treatment, as well as the prevention of suicides and drug overdoses – will be combined with four other agencies to create a new Administration for a Healthy America; staff reductions resulting from that consolidation were not specified, and HHS said that no further cuts were planned.
The New York Times also reports that the Justice Department is considering merging the Drug Enforcement Administration and the Bureau of Alcohol, Tobacco, Firearms and Explosives – a consolidation that would make some logistical sense because many investigations involve both drugs and guns. Some fear, though, the plan might be a pretext for gutting two of DOJ’s smallest and most underfunded agencies.
Meet Therabot, the first AI-powered therapy chatbot to prove its worth in a controlled trial

I’m not a big believer in technological cure-alls. So I was surprised by my reaction to the first randomized controlled trial (RCT) of a generative AI therapy chatbot: I think this technology could be a game-changer for mental health treatment. Not because of the encouraging results from one study published in NEJM AI (one study isn’t enough), or because it could be an equivalent replacement for human therapists (the researchers stress that it wouldn’t be).
Rather, it’s because, as senior author Nicholas C. Jacobson points out in a press release, “there are nowhere near enough providers to go around,” with an average of 1,600 patients with depression or anxiety alone for every available provider in the U.S. Tools like this could fill gaps between provider supply and patient demand.
Therabot, the chatbot studied, has been in the works since 2019. It uses a generative large language model, fine-tuned on conversations drawn up by a psychiatrist, psychologist and other researchers at Dartmouth medical school. The chatbot – represented by an almost comically empathetic-looking avatar – is designed to deliver personalized interventions based on cognitive behavioral therapy, as shown in a demonstration video.
The 210 participants in the RCT, all adults, either had symptoms of depression or anxiety, or were at a clinically high risk for eating disorders. In the first four weeks, the intervention group was prompted to engage with Therabot each day, and over the next four weeks could still use the tool, but were not prompted to. The control group was waitlisted for chatbot access for the full eight weeks. Over that time period, people in the chatbot group with clinical-level symptoms of major depression had a 51% average reduction in symptoms (vs. 27% for controls); those with generalized anxiety disorder reported a 31% decrease (vs. 11% for controls), and participants at risk of eating disorders experienced a 19% average decline (vs. 7% for controls) in concerns about body image and weight. The improvements were “comparable to what is reported for traditional outpatient therapy,” Jacobson says.
Other interesting findings: Users engaged with Therabot for an average of six hours through the eight-week trial, or the equivalent of about eight therapy sessions. They also reported a degree of “therapeutic alliance” – essentially a level of trust and collaboration that is considered essential to successful therapy – in line with what patients report for in-patient providers. For example, their unprompted interactions ticked up in the middle of the night.
During the trial, all Therabot responses were supervised by trained clinicians and researchers post-transmission. Staff contacted participants on 13 occasions to correct inappropriate chatbot responses (like providing medical advice), and ON 15 occasions to provide safety guidance and emergency resources when participants’ comments raised safety concerns (such as suicidal ideation), although Therabot is programmed to show buttons that will call 911 and call or text crisis hotlines as well.
“We did not expect that people would almost treat the software like a friend. It says to me that they were actually forming relationships with Therabot,” says Jacobson, an associate professor of biomedical data science and psychiatry at Dartmouth.
Unique center in Utah offers ‘a warm blanket’ feeling for people in crisis

The Huntsman Mental Health Institute’s new crisis care center near Salt Lake City, based on how it’s described, is beyond anything I’ve come across. The goal of the $64 million facility, which opened on Monday, is to remove any and all barriers to people seeking mental health care.
Money is one of those obvious barriers, and the facility offers 24/7 crisis stabilization to patients whether or not they’re insured, keeping them on site for up to 23 hours with no out-of-pocket costs. Another is knowing where to go – this new facility is open to any and all, a so-called “no wrong door” approach: It has a 24-bed inpatient acute care unit. Outpatient treatment for mental health and substance use disorders, including the medication-assisted treatment (MAT) Suboxone. Case management and coordination with community resources. And legal and dental services run by the University of Utah’s schools of law and dentistry, the Deseret News reports.
Another notable financial fact: the center doesn’t rely on any federal funding other than Medicare and Medicaid insurance – a relief given what’s happening in Washington. Instead, support comes from the state, county, University of Utah, Huntsman Mental Health Foundation and individual donors, particularly the couple for whom the Kem and Carolyn Gardner Mental Health Crisis Care Center is named.
Ross Van Vranken, director of strategy and government relations at the Huntsman Mental Health Institute, told MindSite News that the new center’s model borrowed bits and pieces from designs around the country. The architects (FFKR) sought to create “a warm blanket” feeling for patients (they call them “guests”), with nature-inspired art, a meditation garden, resident-controlled window treatments and an outdoor-facing alcove on the inpatient floor called the “porch,” offering fresh air and a look out onto the grounds. “Giving our guests personal autonomy, serenity, and safety was key,” Van Vranken said.
Utah has the seventh-highest suicide rate in the country – the top 8 states are all in the West – and officials are hoping that the center will help save lives. The new walk-in crisis center is in the Wasatch Front region, home to 75% of Utah’s population, and has triple the capacity of the center it’s replacing. Its short-term crisis support alone is projected to serve over 9,600 unique patients each year.
Suicides fall by 73% after nets are installed at the Golden Gate Bridge

Since the Golden Gate Bridge opened in 1937, more than 2,000 have plunged to their deaths in the waters 200 feet below, far more than at any other bridge in the U.S. Bridge operators there and across the country argued for decades that putting up barriers would make no difference: common sense, they said, suggested that people intent on killing themselves would just find another bridge, or another method.
Research shows otherwise. Multiple studies have found that leaping to one’s death from a bridge – jumping from heights accounts for about 2% of all suicides in the U.S. (as opposed to 52% in Hong Kong) – is an impulsive decision, made out of desperation at one’s lowest point. I discovered that 40 years ago, reporting on suicides from the Delaware Memorial Bridge, which links New Jersey and Delaware. The conclusions from the data and the stories are the same: When people are prevented from jumping, suicides don’t increase elsewhere in the area. When bridge-jumpers survive, they rarely try suicide again.
The Golden Gate Bridge, after years of pushback against suicide prevention groups, finished installing metal safety netting just over a year ago. The nets sit 20 feet below the walkway, extending 20 feet out across 95% of the span. The first study to examine their effectiveness, published in BMJ Injury Prevention, compared suicide numbers before (January 2000 to July 2018), during (August 2018 to December 2023) and after installation (January to December 2024).
The results: The number of suicides averaged 2.48 per month before installation, 1.83 per month during installation and 0.67 per month after installation – a drop of 73% in total.
In other news…
“Dr. Lindsay C. Gibson Thinks Compassion for Our Parents Can Be a Trap,” as the headline on her New York Times Q&A puts it. The headline is succinct and lacking in nuance. In her interview with journalist David Marchese, Gibson – author of the sleeper 2015 best seller “Adult Children of Emotionally Immature Parents” – is anything but.
Discrimination can cause mental health problems. A new study shows just how much. A study of nearly 30,000 adults’ responses to the U.S. National Health Interview Survey in JAMA Network Open analyzed the effects of everyday discrimination, measured as none, low or high on a standardized scale. Compared with no exposure to discrimination, low exposure was associated with roughly double the odds of a positive screening for depression or anxiety, and high exposure with roughly five times the odds. For both depression and anxiety, low exposure was linked to 2.6 times the odds and high exposure with nearly nine times the odds of a positive screening. Associations differed significantly depending on participants’ race and ethnicity.
Black and multiracial people reported experiencing the highest levels of discrimination but whites were less likely to report discrimination and when they did, they were the most likely of all groups to feel depressed.
Anxiety and depression on top of living alone dramatically raise the risk of suicide compared with any of those factors by themselves, according to a large, long-running South Korean study in JAMA Network Open. Living alone with depression was associated with almost four-fold increase in the risk of suicide compared with people who live with others and are not depressed, while living alone with anxiety almost doubled the risk. Living alone with both depression and anxiety was associated with a whopping 558% increased risk of suicide. Out of those living alone with depression or anxiety, those aged between 40 and 64, as well as men of any age, faced the highest suicide risk.
If you or someone you know is in crisis or experiencing suicidal thoughts, call or text 988 to reach the 988 Suicide & Crisis Lifeline and connect in English or Spanish. If you’re a veteran press 1. If you’re deaf or hard of hearing dial 711, then 988. Services are free and available 24/7.
Recent MindSite News Stories
When Freedom Still Feels Like Prison: Life After Solitary Confinement
Solitary confinement can cause severe psychological impacts and the U.N. considers it torture. Yet prolonged isolation remains widespread in U.S. prisons and jails, where more than 122,000 people are held in solitary.
Kendra’s Law in New York: Report Blasts Racial Disparities in Forced Mental Health Treatment
When someone is forced into treatment, it strips them of their autonomy, say critics of Kendra’s Law in New York.
Inside America’s Mental Health Agency: Mass Firings and Work Stoppages Sap Morale
The agency tasked with leading the fight to ease the country’s mental health and addiction emergencies is going through an existential crisis. About 100 of its 900 workers have been fired and those that remain are frightened and demoralized.
If you’re not subscribed to MindSite News Daily, click here to sign up.
Support our mission to report on the workings and failings of the
mental health system in America and create a sense of national urgency to transform it.
For more frequent updates, follow us on Facebook, Twitter and Instagram:
The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.
Copyright © 2021 MindSite News, All rights reserved.
You are receiving this email because you signed up at our website. Thank you for reading MindSite News.
mindsitenews.org

Mental health can't wait.
America is in a mental health crisis — but too often, the media overlooks this urgent issue. MindSite News is different. We’re the only national newsroom dedicated exclusively to mental health journalism, exposing systemic failures and spotlighting lifesaving solutions. And as a nonprofit, we depend on reader support to stay independent and focused on the truth.
It takes less than one minute to make a difference. No amount is too small.
The name “MindSite News” is used with the express permission of Mindsight Institute, an educational organization offering online learning and in-person workshops in the field of mental health and wellbeing. MindSite News and Mindsight Institute are separate, unaffiliated entities that are aligned in making science accessible and promoting mental health globally.










